The Undertreatment of Severe to Profound Hearing Loss: Unlocking the Potential of the Cochlear Provider Network in your Practice
Jennifer LaBorde, Au.D.
Cochlear implants have been the standard of care for adults with severe to profound hearing loss for more than a generation. Recently, the candidacy requirements have become less stringent (Zwolan, Et al 2020); yet utilization rates remain stubbornly low.
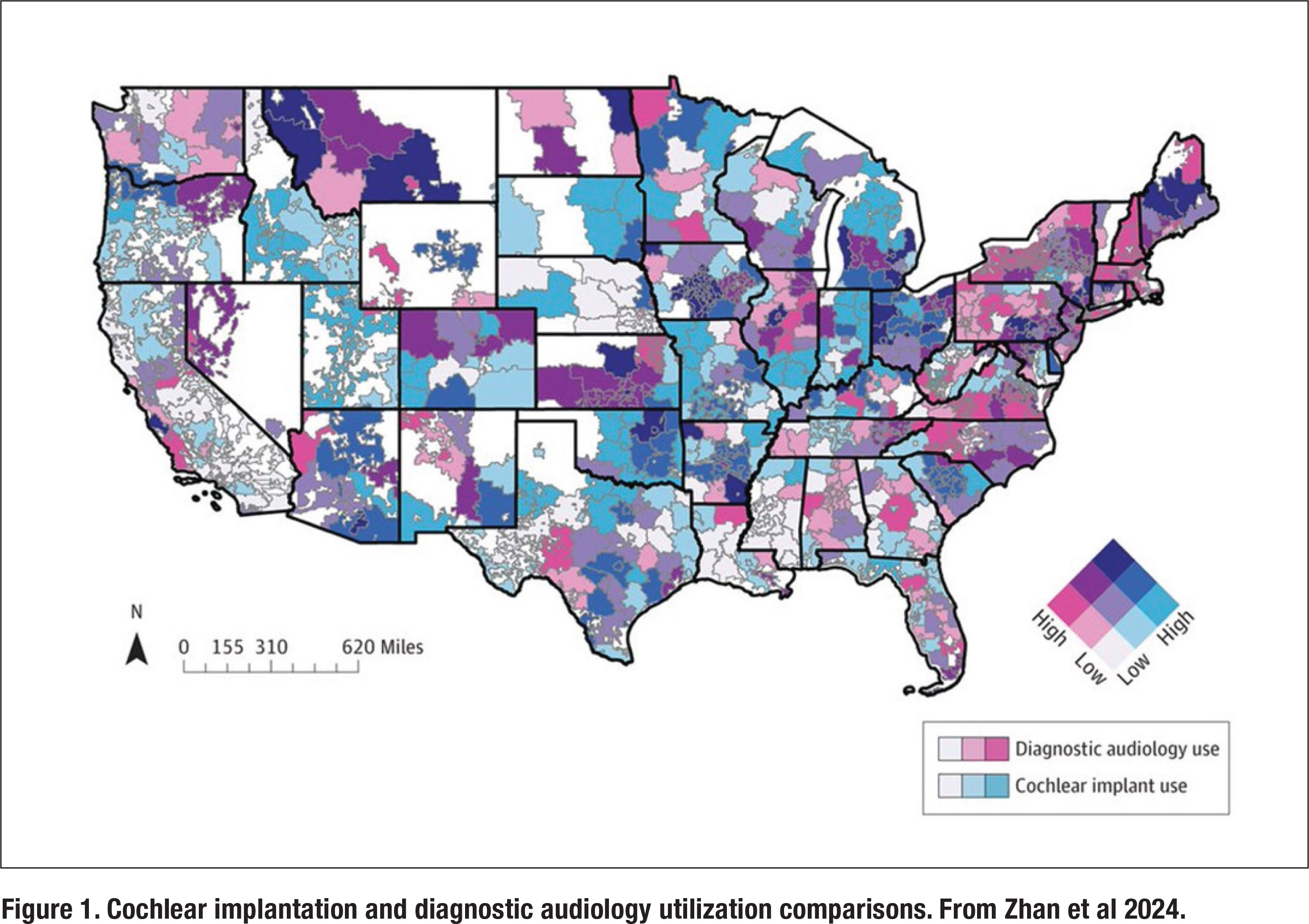
Recently, Zhan and colleagues (2024) used a large medical claims database to better understand the utilization of cochlear implants. Their analysis found that cochlear implant utilization was 0.33% of all patients with sensorineural hearing loss. Utilization of cochlear implants did not significantly correlate with age at diagnosis of hearing loss, audiology utilization, or any socioeconomic variables. As shown in Figure 1, there are large swaths of the US, particularly in the Southeast, where utilization is practically non-existent for both diagnostic audiology and cochlear implantation.
On the other hand, there are parts of the US, namely the Eastern US, Southern California and a few other places denoted in red in Figure 1, where utilization of diagnostic audiology services is high and cochlear implantation is low. This finding suggests that significant under-referral and poor awareness are big drivers of poor cochlear implantation uptake rates. Further, using this data, the authors determined that 5.55% of all adult patients with bilateral hearing loss have severe-toprofound hearing loss, but just 6% of this group (6% of 5.55%) used a cochlear implant. Although the recent loosening of cochlear implant candidacy requirements may not yet be reflected in this abysmally low number, it is clear that severe and profound hearing loss is an undertreated condition.
Given the significant under-referral and poor awareness, combined with the overall low cochlear implantation utilization rates, there has never been a better time to revisit the Cochlear Provider Network (CPN). To better understand how CPN works, is Jennifer LaBorde, AuD, director of audiology at The Hearing Center in Pensacola, Florida.

AP: Tell us about your career journey and your practice.
I have been practicing audiology since 1999, initially in a non-profit Speech and Hearing Center; however, since 2001 I have been employed in a large physician-owned multi-specialty clinic providing audiological services and functioning as department director since 2003. I describe the practice setting as a hybrid ENT/ private practice, as we support a robust ENT practice with complete audiological diagnostic services, but also have a strong focus in audiological rehabilitation services. The practice is entrepreneurial and continuously looking for ways to grow in order to provide services with best practices and an excellent patient experience for our community.
AP: What is the Cochlear Provider Network?
The Cochlear Provider Network (CPN) is a group of audiological practices who do not have in-house cochlear implant surgeons. We provide cochlear implant (CI) services ranging from candidacy evaluation and recommendation for cochlear implants, initial activation of implants, and followup CI mapping services.
AP: How do you position the CPN in your practice (that is, how do you talk about it with patients, how might you advertise it?)
Being a member of the CPN has set our practice apart as a full-service audiological practice from hearing conservation on one end of the continuum to a practice that offers rehabilitative services even for surgical solutions with hearing loss. This full-service continuum elevates the practice in our community as a medical practice offering services beyond a traditional hearing aid. For patients who know that we are trusted partners with the surgeons we refer them to, they feel an immediate and natural trust in our services and abilities.
AP: Take us through the evaluation and treatment process. What are the criteria for a CI evaluation?
Patients who are struggling with speech understanding ability with their traditional hearing devices can be evaluated for a cochlear implant. We accept referrals for cochlear implant evaluations from many sources, including our ENT colleagues, other non-CPN audiologists, as well as patients who self-refer because they have read or heard about the benefits of cochlear implants for improved speech understanding.
We prefer to have a prior audiometric evaluation to ensure that the patient’s hearing ability would be in the range of candidacy. The next step is ensuring that the patients are currently utilizing hearing aids that are set to prescriptive targets. This is typically our starting point for the CI evaluation, as the testing and candidacy requirements are conducted in an appropriately aided condition. Hearing aids would then be adjusted to meet targets, if necessary. Acoustic properties such as dome size or custom earmolds are changed/added in order to meet these prescriptive targets. The patient is then tested in the best aided condition with each hearing aid individually using CNC words to determine if word understanding is poor enough to meet CI candidacy. Further testing is then conducted with sentence material in both quiet and noise to determine a patient’s functional abilities in the best aided condition. Interestingly, patients many times are attending these appointments with hearing aids that are not fit to the patient’s current hearing ability and once verification is performed and necessary adjustments are made, speech understanding improves to above the level that would indicate cochlear implant placement. If it does not, however, I begin counseling the patient on the benefits of cochlear implantation and help them understand the audiological benefits of improved audibility with this type of a device over a traditional hearing aid.
 AP: How does the referral process work?
AP: How does the referral process work?
If the patient is interested in meeting with a surgeon, our practice will refer the patient with their test results and an audiological recommendation for cochlear implantation. The surgeon’s office will then coordinate with the patient what is needed for that surgical consultation. Most times, the patient has an MRI prior to meeting with the surgeon, so that he/she has all necessary information to make a medical determination that cochlear implantation is recommended. And then the surgery is scheduled! It’s quite a simple process for our office, the patient, and the surgeon. The next time the patient will see the surgeon is typically the day they receive their implant!
AP: How does the Cochlear Provider Network benefit your practice?
The ability to provide a full spectrum of audiological solutions to help manage even the most severe impacts of hearing loss as a member of the CPN, we have the benefit and availability of resources such as the Recipient Engagement Manager and Recipient Services Manager. These are people who are employed by Cochlear to aid recipients in their cochlear implant journey, assisting in answering questions about equipment, surgical expectations, and outcomes that a patient may have not remembered or asked during the initial consult with me or their surgeon. These professionals provide support to audiologists and surgeons by taking care of tasks such as helping patients decide on color, style and accessories for their cochlear implant; they provide connections for patients with other recipients who have similar hearing journeys and have been through the cochlear implant process.
AP: Tell us about follow-up and what happens after a patient receives a CI?
Once the patient has had surgery, he/she will return to our office in 3-4 weeks for activation. We have an excellent working relationship with our partner surgeons in the CPN and can communicate with them directly and with ease to address any concerns we might see, which is very rare, otherwise, we can begin activation of the cochlear implant.
AP: Take us through the types and duration of follow-up appointments
This initial activation is typically scheduled for an hour in order to evaluate post-operative hearing status, orient the patient with new equipment, and provide an initial sound stimulation.
The patient then follows up in one month and we measure audibility of sounds, address any sound quality issues, and optimize measurements based on audibility and loudness comfort.
The three-month appointment then consists of re-measuring audibility and now measuring speech perception performance. At this visit, we can review datalogging and continue to optimize MAP settings if necessary. At this point, we can determine if the patient should be scheduled for an annual check, follow up as needed, or return sooner for any specialized concerns that may arise. Most patients are fine to schedule in one year. These appointments are anywhere from 30-60 minutes long.
AP: How do you manage the time needed with longer follow-up appointments? Do you use telecare or audiology assistants?
Cochlear has a wonderful remote care program that allows for both synchronous telehealth mapping as well as an asynchronous remote check of the processor that can be reviewed by the audiologist. This is a great way to triage concerns and address needs in an efficient and expeditious way. Our office also utilizes our audiology assistants for equipment troubleshooting and triaging to empower patients when they need to directly contact the cochlear implant manufacturer or truly need to be seen by an audiologist.
AP: What CPT codes can be used for CIs in adults?
I am certainly no coding expert, but we utilize codes for diagnostic analysis of cochlear implants for both initial and subsequent reprogramming (92603 and 92604 for those older than 7 years). We utilize the evaluation of auditory rehabilitation status codes for candidacy evaluations as well as speech perception testing, validation measures, and counseling on the implication of the results with the cochlear implants (92626 and 92627, both of which are time-based codes).
AP: At a high level, what are the typical reimbursement rates for these CPT codes?
Generally, reimbursement rates for these codes are typically covering the time spent for the procedures, however the transition from hearing aids to cochlear implants does require a learning curve for both patients and providers. Nearly all patients and providers are accustomed to bundled devices and professional services, but with cochlear implants, insurance does not reimburse for our time assisting with equipment troubleshooting and rehabilitative services for these patients. Clinics can handle this in a variety of ways, such as charging per service or implementing a service plan for these types of encounters so that patients experience a similar level of access to our services as they were likely accustomed to with hearing aids.
AP: What support does Cochlear provide for the CPN providers?
Another way to help provide ongoing support to our patients is using the CPN resources that are available such as the Recipient Service Managers. These professionals can assist patients with orientation of their equipment, finding ways to utilize listening accessories, and even assisting patients with upgrade equipment when necessary.
Cochlear also has community engagement events for potential recipients to help answer questions for patients considering cochlear implantation. Further, should an audiologist want to being offering cochlear implant services, Cochlear provides consistent, reliable support to help implement these services into the practice, provide continuing education and support for providers to feel confident, and provide real-time assistance from audiology on-call services and remote assistance during patient encounters.
AP: How can other practices get involved with the CPN?
Contacting Cochlear directly is the best way to get involved with CPN. For our office, being a part of the CPN has been a great collaboration with surgeons in our region and allowed us to offer continued hearing care services to our patients when amplification is no longer providing adequate benefit. You can find all you need to get started with the CPN at cochlear.com. ■
References
- Zhan KY, Mazul A, Kallogjeri DL, Buchman CA. Use of Diagnostic Audiology and Cochlear Implantation in the US. JAMA Otolaryngol Head Neck Surg. Published online February 22, 2024
- Zwolan TA, Schvartz-Leyzac KC, Pleasant T. Development of a 60/60 Guideline for Referring Adults for a Traditional Cochlear Implant Candidacy Evaluation. Otol Neurotol. 2020;41(7):895-900.
Dr. LaBorde, originally from Lafayette, LA, moved to Florida in 1999 to begin her career in audiology. She obtained her doctor of audiology degree from the University of Florida, master’s in communication disorders from the University of South Alabama, and bachelor’s of science in communication disorders from the University of Mississippi. She can be contacted at
