Elements of a Strategic Plan: Implementing Hearing Screenings during Health and Wellness Appointments for Individuals 55 years and Older
Lexi Rozycki
It is often said that hope is not a strategy. Even though most audiologists do not have any formal business training, it is a mistake for them to simply hope their business operation will improve. That is where careful, deliberate, and systematic strategic planning comes in. Strategic planning, when completed periodically, requires us to look into the future and use data, often collected from numerous sources, to create a plan that will narrow a financial gap, start a new program, or improve the performance of some existing element of the business.

This case study is one such example of how strategic planning can be used to create a new revenue stream – one that taps into an unmet need of the market that could be better served by an audiology practice. It is meant to serve as an example of how entrepreneurial audiologists can do more than hope; they can create a plan and then work the plan they have created. Let this case study serve as a template for others who may be looking to expand their practice or close a service gap in their community.
The Executive Summary
Miami Multispecialty Clinic has been a staple of the community since 1987. Over the years, the relationship between patients and providers has only grown and has allowed for the quality patient care to improve. However, based upon customer reviews and feedback, there is room for the company to grow and excel even further. Current patients report there is a deficit in the interprofessional relationship regarding the care they receive from several of the departments with our clinic. This statement is supported by Net Promoter Score data, collected over the past three years. The number of net promoters of our practice (those circling an 8-10 on a satisfaction survey) has dropped from 82% in 2020 to 74% in 2023.
As the largest multispecialty clinic in southern Florida, doctors and clinical professionals should have stronger relationships and a better internal referral system between departments. We believe improving this referral network will improve the Net Promoter Score. Within the Audiology department of the Miami Multispecialty Clinic, we believe we can improve transitions of patient care from the primary care provider (PCP) to the Audiology department. By training PCPs on the importance of hearing health and providing a specified room for hearing screening for patients coming from PCP appointments for a screening, we believe we can not only increase clientele for the Audiology department but improve the quality of life of the aging population.
Mission Statement of the Miami Multispecialty Clinic Audiology Department
To provide high quality hearing/balance testing and treatment as part of a holistic healthcare plan derived by an interdisciplinary team in a singular and convenient location for individuals regardless of any and all cultural backgrounds.
Target Customers and Industry Analysis
Age-related hearing loss (presbycusis) is a common factor associated with aging. There have been studies linking hearing loss with diabetes, vascular disease, depression, stress, and social isolation (Souza 2014).
With healthy aging, there is often cognitive decline that results in a decrease of long-term memory, working memory (processing and storage during listening), processing speed (time necessary to evaluate and assign meaning to changing acoustic signals), and executive function (ability to direct attention and ignore extraneous information). All these cognitive processes are vital to communication. In addition to aging, these factors can decline more rapidly when there is a hearing loss. Additionally, there has been epidemiology data that has shown hearing loss is associated with an increased risk of cognitive decline and/or dementia. The association persists even after controlling for hearing related conditions (Souza 2014).
Despite the known risks associated with age related hearing loss, the average time it takes for an individual to seek an appointment after noticing a decline in their hearing is about seven years. Additionally, the average age of first-time hearing aid users is 70 years old (Adirondack Audiology 2020). However, there is a significant portion of the population who will experience a hearing loss before they seek out a hearing examination or hearing aids. Table 1 below lists prevalence data of the percentage of hearing loss with different age demographics:
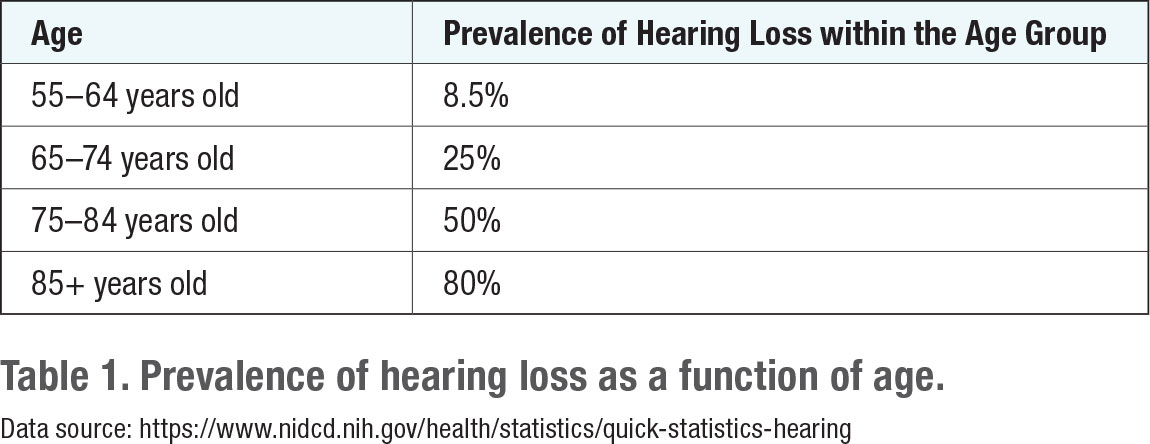
 Due to time constraints and a general lack of knowledge, PCPs often play a minimal role in hearing loss identification and treatment (Souza, 2014). By implementing hearing screening during routine PCP appointments once a year for individuals 55 years of age and older, with no identified hearing loss, Miami Multispecialty Clinic Audiology Department will be able to assist the aging population when hearing loss initially begins to occur. We believe this will help minimize health-related risk factors associated with hearing loss and increase the quality of life for patients who decide to forego treatment for hearing loss.
Due to time constraints and a general lack of knowledge, PCPs often play a minimal role in hearing loss identification and treatment (Souza, 2014). By implementing hearing screening during routine PCP appointments once a year for individuals 55 years of age and older, with no identified hearing loss, Miami Multispecialty Clinic Audiology Department will be able to assist the aging population when hearing loss initially begins to occur. We believe this will help minimize health-related risk factors associated with hearing loss and increase the quality of life for patients who decide to forego treatment for hearing loss.
During a recent monthly staff meeting, the Miami Multispecialty Clinic Audiology Department conducted a Strengths, Weaknesses, Opportunities and Threats (SWOT) analysis in which all team members participated in creating. Note that this SWOT analysis was essentially a brainstorming session in which staff, lead by the department’s director, agreed on the various outcomes summarized in Figure 1. The results of the SWOT analysis are shown in Figure 1.

Implementation Strategy
To create a referral service from the PCP department to the Audiology department. Audiology staff listed a series of steps that need to be completed:
- Purchase Equipment and Set up Screening Area
- Area for Screenings
- Unused exam room on the first floor of the Audiology department.
- The exam room already contains an audiometer for screenings.
- Unused exam room on the first floor of the Audiology department.
- Equipment needed for screenings:
- Audiometer and supra-aural headphones
- Otoscope and Speculums
- Area for Screenings
- Conduct Training Session for PCPs
- Lunch & Learn with PCPs
- Creation of Material to inform PCP on the importance of hearing screenings, and how referrals will benefit their patients.
- Have one audiologist lead an hour-long lunch and learn to train PCP and begin implementation of PCPs.
- Lunch & Learn with PCPs
- Hire and Train a Lab Technician to Complete the Hearing Screenings
- A lab technician can be trained to implement hearing screening effectively. This would be their primary role, as well as documenting those who need to be contacted by supporting to set up a hearing evaluation.
- Hire an Audiologist to support the influx of patients from the hearing screenings
- Due to a steady increase of new referrals from the screening program, a new audiologist will need to be hired to meet demand.
- Implement Coding and Billing Revenue Model
- PCP will need to refer and bill for a hearing screening during their appointments.
- CPT 92551: “Screening test, pure tone, air only”
- Medicare does not reimburse for screenings.
- CPT 92551: “Screening test, pure tone, air only”
- If a hearing screening is failed, there will need to be a hearing evaluation.
- CPT 92557: Comprehensive audiometry threshold evaluation and speech recognition
- If there is a hearing loss, the patient will likely need to purchase hearing aids.
- PCP will need to refer and bill for a hearing screening during their appointments.

Estimated Revenues
To begin calculating potential financial projections, we need to determine the demographic of the aging population. Table 2 below breaks down Miami’s population into four main age demographics (55-64 years, 65-74 years, 75-84 years, 85+ years). Next, we isolated the percentage of individuals with a hearing loss based on the Miami population data categorized by age. The following percentages were used to determine how many patients would have not been identified with and treated for a hearing loss if not for the PCP hearing screening referral program.
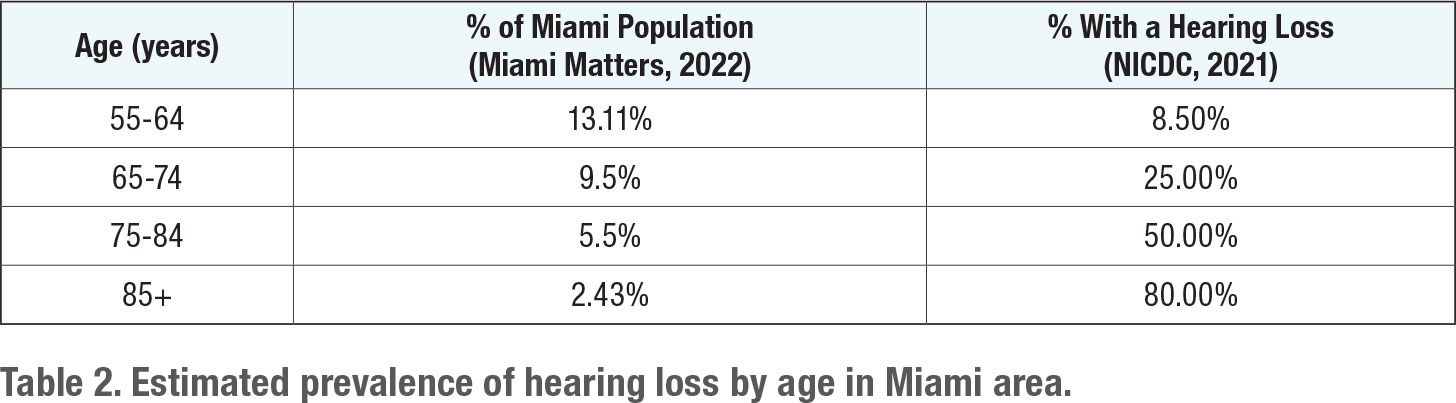
The following calculations are based upon the number of PCP patients seen within the multispecialty clinic. An average multispecialty clinic ranges from 12-20 PCPs. In the Miami area, the average clinic has ~15 PCPs, which will be the number used for this analysis. Per PCP, the number of patients they see per year is 1500-2000 people. This allows for a range of 22,500-30,000 seen by a single multispecialty clinic.
Additionally, 15-20% of adults who could benefit from hearing healthcare services are currently not receiving them. (Dubno et. al., 2022). This number will be important when determining the number of patients being seen who have a hearing loss and are being treated versus those who are unidentified and not being treated for a hearing loss. For this scenario, we will be using the low end of the estimate, 15% when making our estimates.
Next, we estimated the total number of patients seen in the clinic who are 55 years of age and older, and the total number of the individuals likely to have hearing loss. We started with taking the percentage of each age group of the Miami population and multiplying it by our population size, 22,500, to estimate the number of patients in each age group that we see in the clinic. From here, each age group is multiplied by the demographic of the percentage of individuals in each age group who are anticipated to have a hearing loss.
These estimates are shown in Table 3.
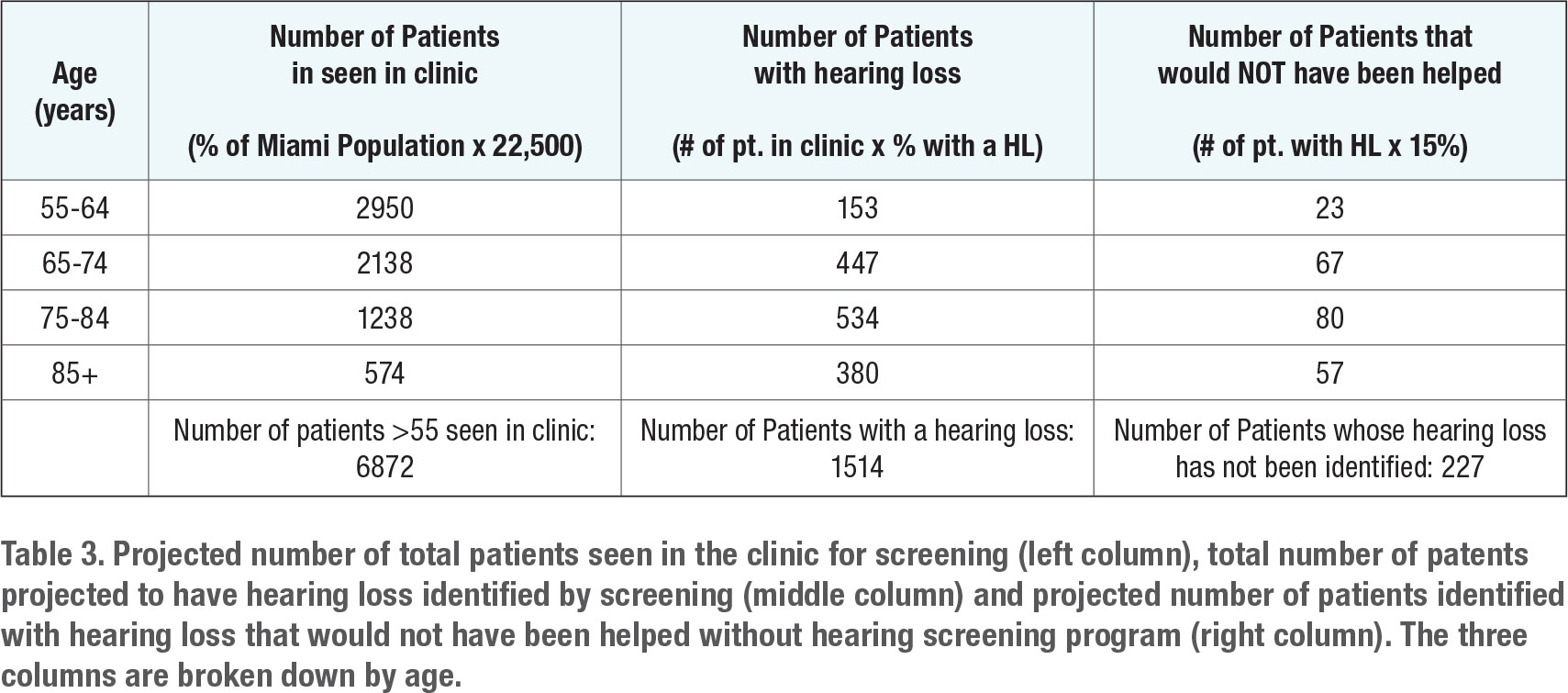
We now have the number of patients aged 55 years and older seen in the clinic by a PCP, those with a hearing loss in that group, and the number of those who do not know they have a hearing loss, but were identified because of the hearing screening program. From this, we can start calculating the number of patients who need to be screened. When looking at who needs to be screened, we only want to screen those who do not have a known hearing loss. We can get this number by calculating the following:
(# of pt. 55> seen in clinic) – (# of pt. with a HL - # of pt. whose HL has not been identified) = # of pt. with known HL
(6,872) – (1841-227) = 5308 patients who need to be screened per year
The number of patients who need to be screened each year is estimated to be 5308. For each screening, we are anticipating it takes approximately 15 minutes (10 minutes to screen and 5 minutes between patients). The following calculations are based upon this number.
(8 hours in a working day) x (60 min. in 1 hour) = 480 working min. in a day
(480 working min.) x (260 working days in a year) = 124,800 working min. per year
(124,800 working min. per year)/ (15 min. per screening) = 8320 possible screenings per year
(approximately 32 screening per day)
With one employee acting as the sole hearing screener, it would be feasible to screen 5308 patients, as in theory, there are enough clinical hours available per day to screen 8320 patients.
Now let’s look at the clinic’s projected compensation for conducting these hearing screenings. Private insurance and Medicare does not cover the cost of hearing screening for patients. This means, for each screening, we would be charging out of pocket and collecting the money after the screening. Based upon research completed by Dubno et.al. in 2022, the average cost of an in-clinic PCP referral hearing screening was $31.64.
(5308 patients screened) x ($31.64 per screening) = $167, 945 per year
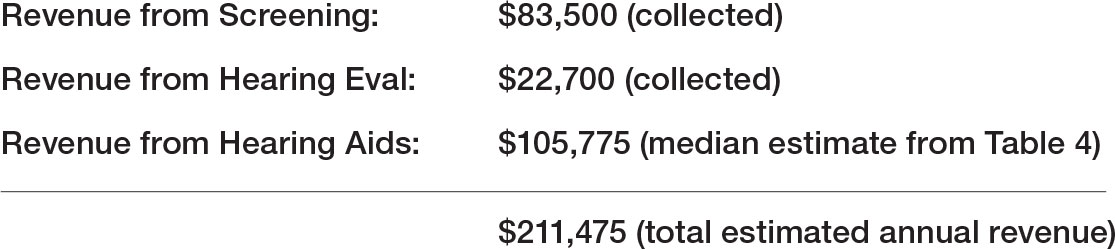
Based upon hearing screenings alone, the projected billed revenue would be $167,945 per year. Further, we are projecting that just 50% of this revenue from hearing screening will be collected. This yields a projected collected revenue figure of $83,500.
We believe that additional revenue will result from the sale of hearing aids that come from patients who fail the hearing screening and then opt to be evaluated by the Audiology department. Consequently, we calculate potential revenue from the hearing evaluations and hearing aids sold to the population that has failed the screening (estimated to be 227 patients). In the clinic, an annual hearing evaluation is covered by most private insurances and Medicare. The revenue per patient is estimated to be $100 per patient. Based upon this projection, we can calculate the gross revenue from hearing evaluations from the 227 unidentified patients:
(227 unidentified patients with hearing loss) x ($100.00 per hearing eval.) = $22,700 per year
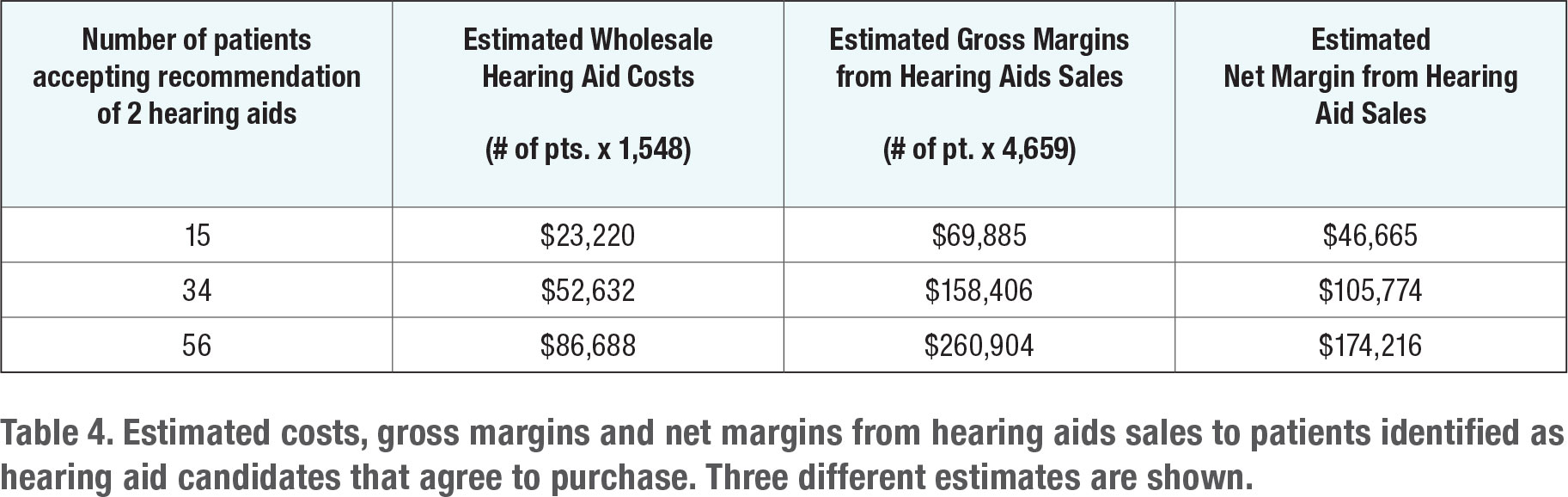
From here, we can assume a portion of these patients will purchase hearing aids. In Table 4, we have three projections of the number of patients who fail the hearing screening, and then agree to purchase hearing aids from the Audiology department.
When estimating potential hearing aid revenue, the following benchmarks were applied:
- Average Wholesale Hearing Aid Cost (2 hearing aids/bilateral fit): $1,548.00
- Average Retail Hearing Aid Cost (2 hearing aids/bilateral fit): $4659.00
- Note the projections in Table 4 are based on a bilateral fit rate of 100%.
Now, we estimate the total revenue from the PCP hearing screening referral program for one year. It shows revenue streams from three sources: the screening, the hearing evaluation, and the sale of hearing aids. Note that we are estimating the amount of collected revenue and expect about one-half of the revenue, coming from the screening portion of the program, to be written off and uncollected.
Estimated Costs to Start Program
We plan to hire a hospital technician for the hourly rate of $18 per hour to complete the screenings. Included in the cost of labor, shown in Table 5, is total compensation, including wages and cost of healthcare insurance for the newly hired technician. The total projected cost for labor for the first year is $42,000. All the projected start-up costs are shown in Table 5.
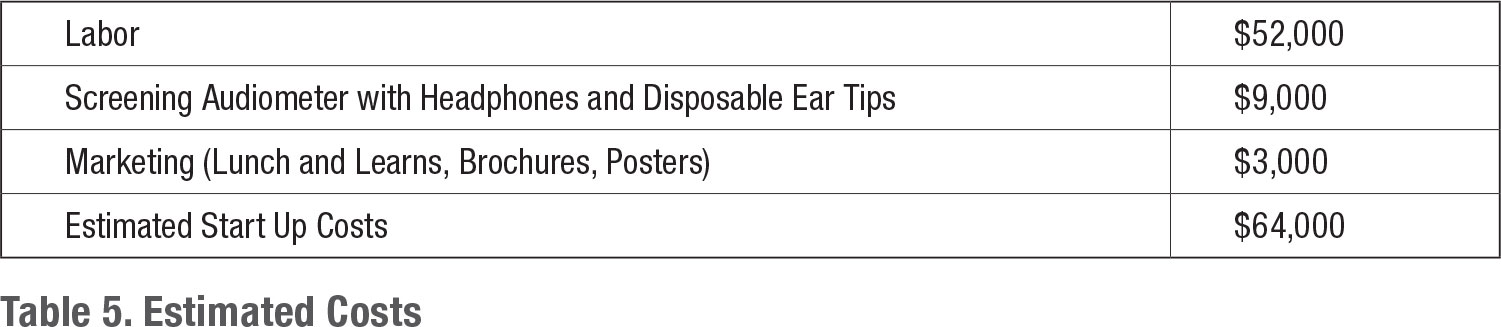
Marketing Plan
Because the entire program is contained within the same multispecialty clinic, marketing costs are nominal. The $3,000 marketing budget is mainly used for the creation of posters, brochures, and other printed material needed to educate staff and patients. There will be an initial training session with the PCPs devoted to the importance of routine hearing screenings for those 55 years of age and older. The cost for the lunch and learn sessions that educate PCPs and staff is also factored into the marketing budget.
As for raising awareness for patients coming into the clinic, we believe through the lunch and learn trainings, PCPs will be able to adequately explain the reason behind the screening program (and why it is beneficial to the patient’s health) to PCPs and their staff members. From there, we believe that after the screening, the audiologist can reinforce the importance of treating hearing loss at early stages of onset.
Although no marketing cost is accrued for it, a significant part of our overall marketing strategy is sending concise, timely reports to the referring PCP after each patient encounter with Audiology. We believe this process will build high levels of trust between the PCP and the Audiology department that will result in fewer marketing dollars being spent in later years.
Expected Obstacles Anticipated and Plans to Overcome Them
There are few anticipated obstacles related to achieving these projected financial goals. Even if there are fewer hearing evaluations and hearing sales then projected, the clinic would not lose money by continuing the hearing screening program.
 PCPs may be hesitant to refer every patient 55 years of age and older for a hearing screening, especially if there are no current concerns for their hearing. To overcome this, we believe that training is a critically important aspect of the start-up process. Emphasizing the difference between the degrees of hearing loss, and how treatment at any level can help improve overall health and quality of life would help ease resistance that may come from the PCPs.
PCPs may be hesitant to refer every patient 55 years of age and older for a hearing screening, especially if there are no current concerns for their hearing. To overcome this, we believe that training is a critically important aspect of the start-up process. Emphasizing the difference between the degrees of hearing loss, and how treatment at any level can help improve overall health and quality of life would help ease resistance that may come from the PCPs.
We plan to closely monitor the number of patients, aged 55 years and older seen by the PCPs, compared to the number of those patients who have their hearing screened. Our goal is to screen 90% of all patients aged 55 years and older. At the end of the year, if we fall below that number, we may add a measure of auditory wellness, the Hearing Handicap Inventory – Screening (HHI-S) version to the protocol. Adding the HHI-S would allow us to pivot away from conducting hearing screenings on all patients and simply administer a questionnaire to them. If we pivot away from traditional pure tone hearing screenings and conduct fewer of them, the technician would be cross-trained as an audiology assistant.
Perhaps a more significant obstacle are patients who fail the initial hearing screening and choose to not participate in any follow up care with Audiology. To reduce the chances of no-show appointments with Audiology, the technician will automatically schedule follow up appointments on the day of the hearing screening for those who fail it. Additionally, no-show appointments will be flagged, and a report will be sent to the PCP’s staff encouraging them to follow-up with each patient who fails.
To maximize the number of patients served, education on hearing loss and how it affects their physical and mental health is very important. We want patients to make informed decisions about their health, and we want to educate patients. This is a process that begins in the PCPs office, at the hearing screening. An additional strategy that could be implemented is handing out printed information for those who fail the hearing screenings on the risk factors associated with hearing loss, and how hearing aids will be able to help mitigate these factors.
Conclusions
The PCP Hearing Screening Referral Program fulfils the mission of interdisciplinary teamwork between departments by serving the aging population of Miami, Florida. The program will not only positively impact patients, but also provides additional new revenue through the sale of hearing aids to patients who ordinarily might not seek care. ■
References
- 2022 Demographics: Age Data for County Miami-Dade. (2022). Miami Matters. https://www.miamidadematters.org/demographicdata?id=414§ionId=942
- Dubno, J. R., Majumder, P., Bettger, J. P., Dolor, R. J., Eifert, V., Francis, H. W., & Tucci, D. L. (2022). A pragmatic clinical trial of hearing screening in primary care clinics: cost-effectiveness of hearing screening. Cost Effectiveness and Resource Allocation, 20(1), 26.
- Quick Statistics About Hearing. (2021). National Institute on Deafness and Other Communication Disorders (NIDCD). https://www.nidcd.nih.gov/health/statistics/quickstatisticshearing#:~:text=One%20in%20eight%20people%20in,based%20on%20standard%20hearing%20examinations.&text=About%202%20percent%20of%20adults,adults%20aged%2055%20to%2064
- Souza, P. E. (2014). Hearing loss and aging: Implications for audiologists. ASHA. https://www.asha.org/practice-portal/professional-issues/adult-hearing- screening/
- What Should You Know Before Buying Hearing Aids?. (2020). Adirondack Audiology. https://adirondackaudiology.com/what-should-you-know-before-buying-hearing- aids/
Lexi Rozycki is an Au.D. Student at the University of Wisconsin. She can be contacted at
