Registration Help

Your partner in your success
Master Studio
As a master studio we can offer opportunities in the Webcam industry and video creation
Start or continue your career here.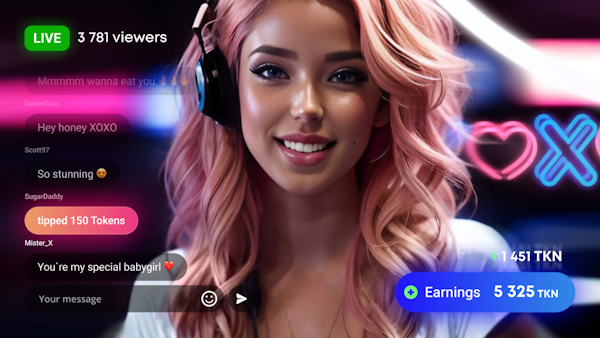
Experienced | Seeking Representation | Very Experienced
A Private show is your chance to communicate with viewers in a more intimate, one-on-one way. It is your best bet to become the focus. In order to start a Private show with the model, the viewer simply presses the “Start Private” button.
As a Webcam modelYou have the opportunity to engage in vibrant and stimulating conversations with adult viewers. Through one-on-one chats, you can establish a more personal connection with your audience, creating a sense of satisfaction and eliciting positive sensations such as relaxation or pleasure.
TrainingWith the guidance of our experienced management team, you will receive training on our software and valuable insights on how to excel in the competitive adult entertainment industry. Our goal is to equip you with the necessary skills and knowledge to thrive in this dynamic field, ensuring your success as a live chat model.
Share in advertising revenue on your videos on major porn sites. Our studio produces your video and distributes to help you get noticed. Through our comprehensive training, support services, and industry expertise, we empower our models to thrive and succeed in their roles. Join us at Luxe Model Collective and embark on a rewarding journey in live chat and adult content creation.
Model News
Frequently Asked Questions
LoyalFans creators can connect through Subscriptions, single pictures/picture sets, clip sales, post tips, referral programs, voice messages, personal requests
Our Spotlight




Visit Our Boutique