
Implementing Block Scheduling: Work Smarter, Not Harder
Zach Malone and Ron Patton
The goal of this case study is to demonstrate the utility of block scheduling and how it helps a practice better manage time spent generating revenue.
Block scheduling is a method of creating a work schedule in which the workday is divided into blocks of time and each block is assigned a specific type or sub-type of activity. This framework not only ensures that critical, revenuegenerating tasks are given the necessary resources to be completed, but it also provides an infrastructure to quickly alert management if a clinician or practice is falling short of projected to financial targets.
What is block scheduling?
Block scheduling is a method of creating a work schedule in which the workday is divided into blocks of time and each block is assigned a specific type or sub-type of activity (i.e. hearing aid evaluation, private pay hearing aid evaluations, third-party hearing aid fitting fee, check & clean, outbound calling, etc.). The level of detail for each block category can be tailored to an individual practice, but the overarching goal of block scheduling remains constant: To ensure there is necessary time to complete a given business activity and to safeguard that each clinical task is completed in a way that meets business objectives. Completing revenue-generating activities in a timely way, while setting aside sufficient time to complete other necessary work that keeps the practice operating smoothly, is referred to as efficiency. At its core, block scheduling is a proven way to efficiently manage time, a practice’s most precious resource.
To clarify the point that time is a practice’s most precious resource, let’s review an example. Say that a practice has significantly increased the number of patients it has seen this year, compared to the previous year, but the amount of revenue has decreased. A likely cause of this revenue shortfall is the increased use of third-party insurance contracts, which tend to have smaller gross margins. As this case study attempts to demonstrate, the use of block scheduling is an effective strategy that manages this common challenge.
The block scheduling process enables a practice to attain business goals by being more efficient with how time is spent. Appointment time is set aside for appointments that tend to generate ample revenue. Additionally, this process of establishing block schedules breaks down the important annual financial goals into the daily necessary steps or subgoals. Because the annual revenue goals are broken down into daily subgoals, managers will quickly be alerted to any deviations to the plan. With the alerts being executed in real-time, management can quickly take corrective actions to get the business back on track to meet goals.
Another helpful practice that uses similar mechanics to block scheduling is called reverse block scheduling. This process helps limit specific activities that, when in overabundance, can hinder or prevent a practice from meeting its financial goals. One example of reverse block scheduling is capping the number of hearing aid evaluations involving third-party contracts or hearing aid check-ups, which generate less revenue, to a certain number per week. Of course, all patients are important, but a practice must balance financial solvency with other commitments that serve the needs of the entire community. The use of reverse block scheduling (capping the number of low-revenue appointments each week) ensures there is sufficient time on the schedule for more lucrative private pay opportunities.
Let’s examine how different types of revenue-generating appointments affect net revenue. Figure 1 shows a breakdown of Clinic X’s revenue for the past four years. Comparing 2021 to 2018, the managers were surprised to find that despite an 88% increase in the number of hearing aids fit, the total revenue has dropped by almost 3%. The practice manager can observe from the financials shown in Figure 1 that the disappointing revenue number comes from a combination of a higher percentage of fitting fee patients and a declining average selling price per hearing aid. Note that fitting fee revenue is generated from third-party contract sales.
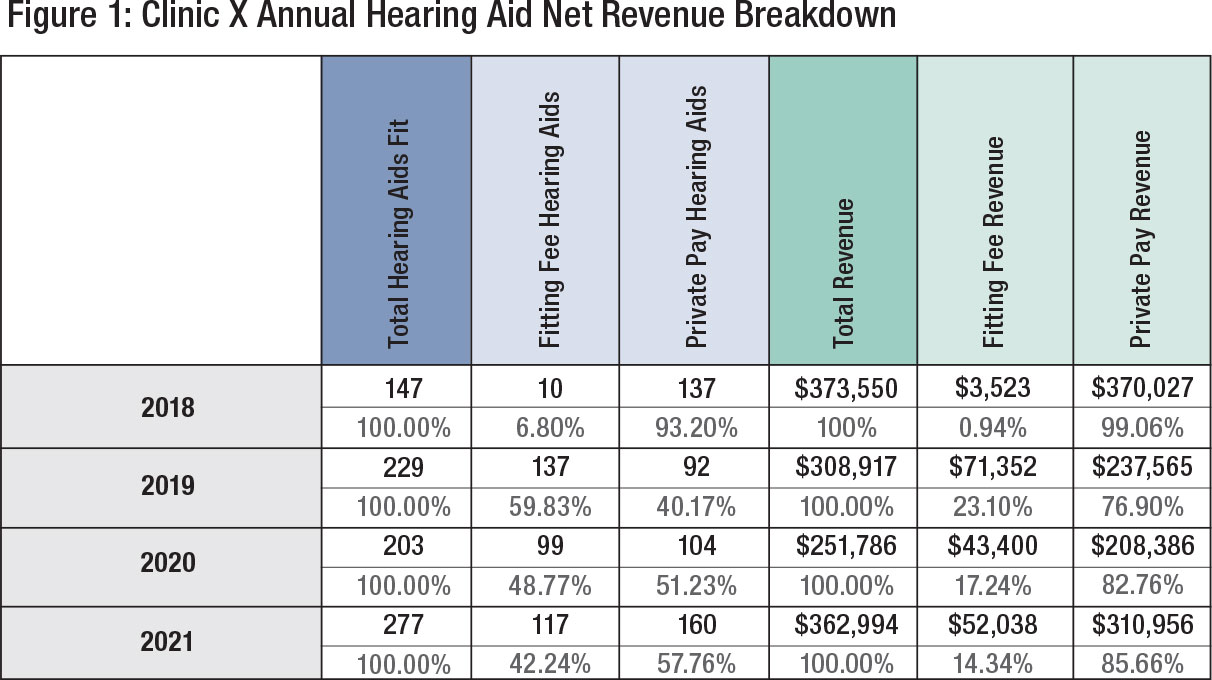
The managers in this practice are aware of tactics to improve the average selling price but wanted to implement block scheduling to mitigate the increasing number of patients using third-party payment options to ensure they would meet revenue targets. Moreover, the managers wanted to develop a plan for identifying when the practice falls short of revenue targets throughout the year. The goal being to allow for enough time to make any adjustments to operational tactics (e.g., monthly promotions, new marketing programs) with sufficient time to execute these changes in plans.
Next, we demonstrate in a step-by-step manner how a block scheduling approach with the goal of optimizing revenue from the sale of hearing aids was implemented in this practice.
Step 1: Block Scheduling Pre-Work
Prior to implementing a block schedule, the practice manager must gather the necessary datapoints outlined in Figure 2.
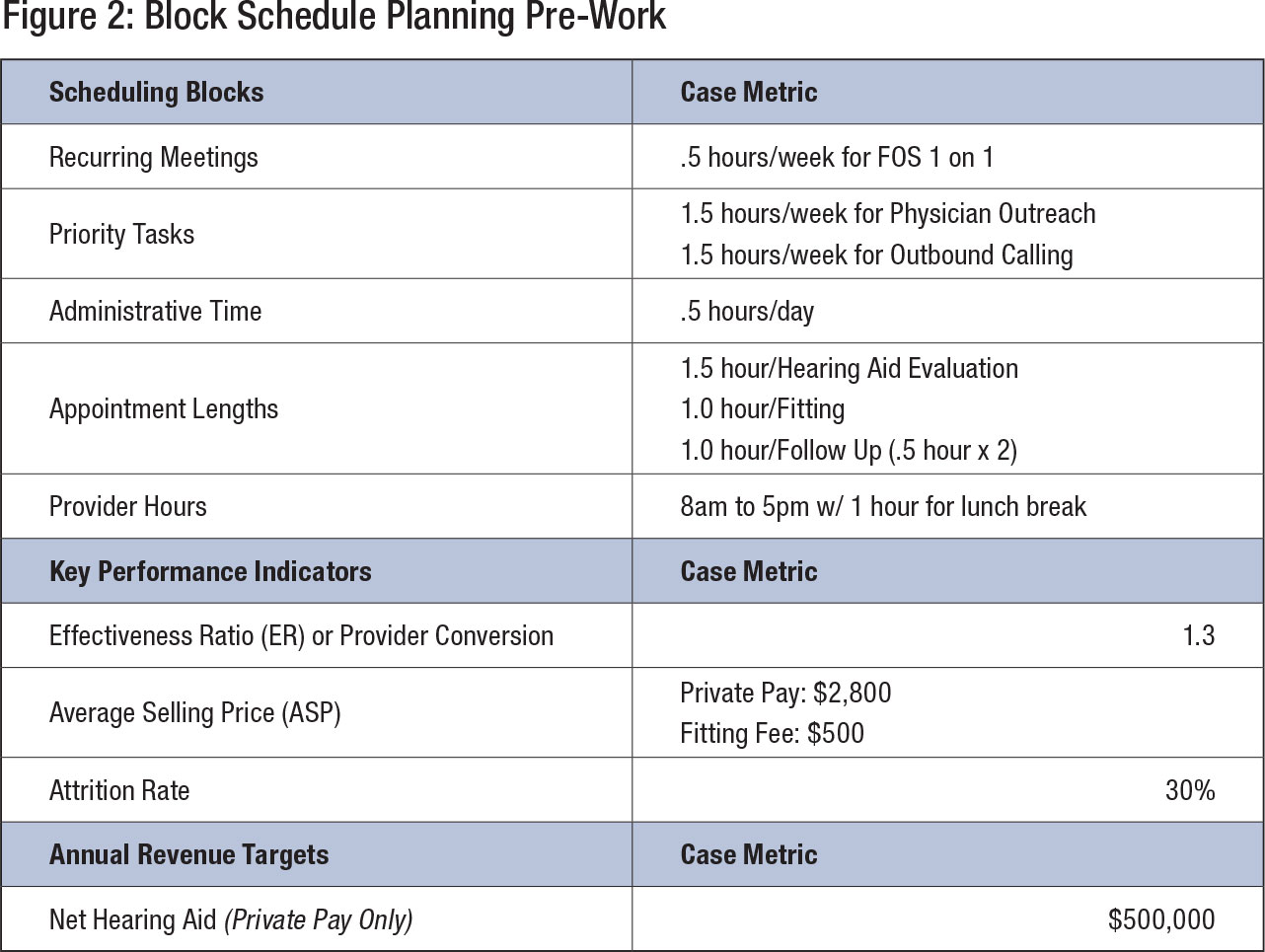
Recurring Meetings are those necessary scheduled staff interactions that occur on a regular cadence. Because these meetings are necessary to the business function, a block of time should be reserved on the schedule to ensure they will occur as needed. In the instance of this case study, the manager has dedicated 30 minutes a week for a 1-on-1 meeting with the front office Patient Care Coordinator.
Priority Tasks are those necessary tasks that occur on a regular cadence. Because these tasks are necessary to the business function, a block of time should be reserved on the schedule to ensure they will occur as needed. In the instance of this case study, the manager has dedicated 1.5 hours a week for Physician Outreach and 1.5 hours a week for Outbound Calling.
Administrative Time gives a provider the opportunity to catch up on patient notes. Since each patient’s needs and appointment circumstances are unique, allotting time to making sure a patient’s record and subsequent databases are up to date will ensure smooth business operations and minimize negative impacts to the business operations. In the instance of this case study, the manager has dedicated 30 minutes each day for Administrative Time.
Appointment Lengths are the length of time it takes to treat a patient for a specific need. In the instance of this case study, the manager has allotted 1.5 hours/hearing aid evaluation, 1.0 hours for hearing aid fitting and two 30-minute follow up appointments per patient.
Provider Hours are the hours in which patients are seen by providers. In this case study, the manager has determined patients can been seen between the hours of 8am and 5pm with a one-hour lunch break from 12:00 p.m. to 1:00 p.m.
Effectiveness Ratio (ER) or Provider Conversion is the rate at which a patient with a treatable hearing loss or condition agrees to move forward with amplification as part of their treatment plan. This metric can be calculated by dividing the number of hearing aids fit by the number of opportunities seen. The highest ER a provider could receive is a 2, because a provider can fit a typical treatable patient with 2 hearing aids (1 for each ear). In the instance of this case study, the Effectiveness Ratio is 1.2, meaning the provider fits, on average, each treatable patient with 1.2 hearing aids.
Average Selling Price is the mean price paid per hearing aid, inclusive of any bundled service (i.e. hearing aid evaluations, fittings, follow ups, clean & checks). In the instance of this case study, the manager’s ASP for a patient utilizing private pay at $2800. The manager has opted to not take third party or fitting fees, because the ASP has historically been a small fraction of private pay.
Attrition Rate is defined as the rate at which a scheduled appointment does not result in a treatable patient. Attrition can happen for several reasons, but predominantly include: 1) The patient cancels the appointment without rescheduling and the previously reserved time slot cannot be filled, 2) The patient unexpectedly does not show up to the appointment, or 3) The hearing aid examination concludes the patient does not require treatment. In the instance of this case study, the attrition rate is set at 30%.
Net Hearing Aid Revenue Target is the revenue target minus any refunds, returns or discounts. A best practice for calculating this number is to work with a financial planner or CPA to protect against setting a revenue goal that will exceed business expenses and account for the desirable level of profitability.
Step 2: Calculating the Targets
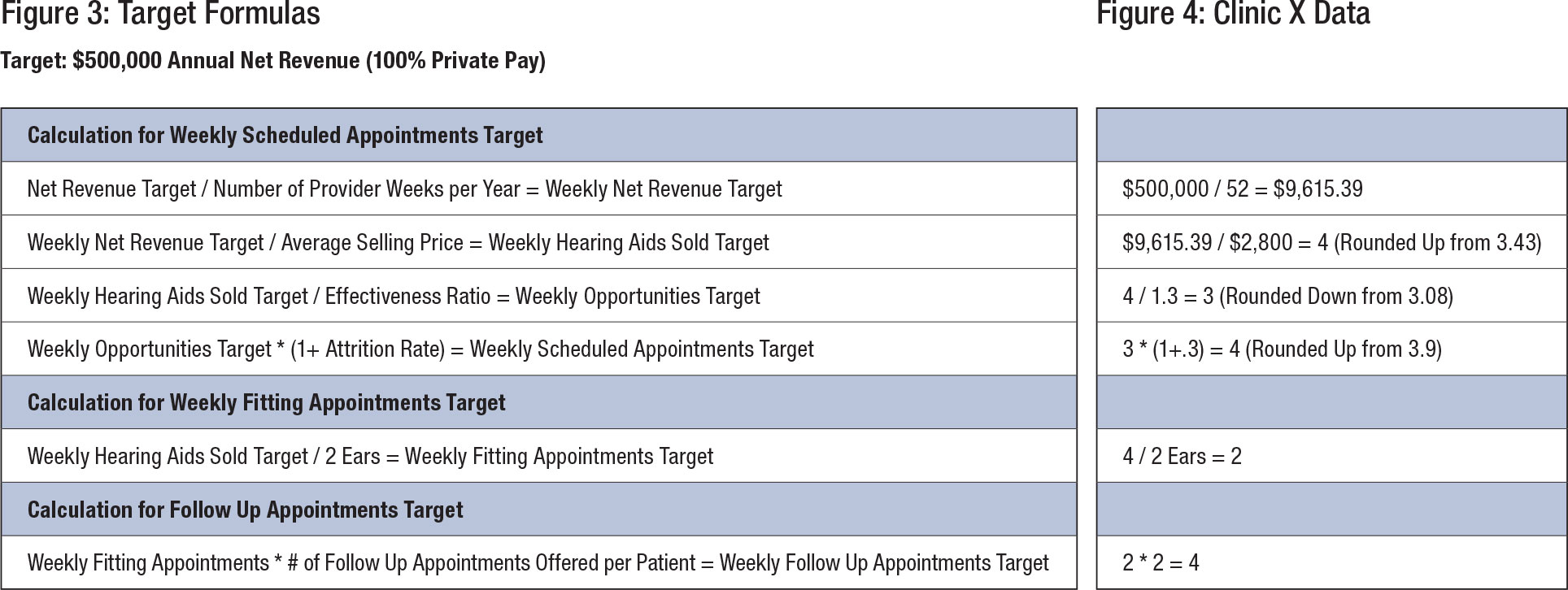
Once the datapoints are collected in Step 1, they are used to complete the calculations for the following targets in Figure 3: Weekly Scheduled Appointments, Weekly Fitting Appointments, and Follow Up Appointments. Figure 4 shows the results of these calculations with the datapoints completed.
Step 3: Creating the Block Schedule
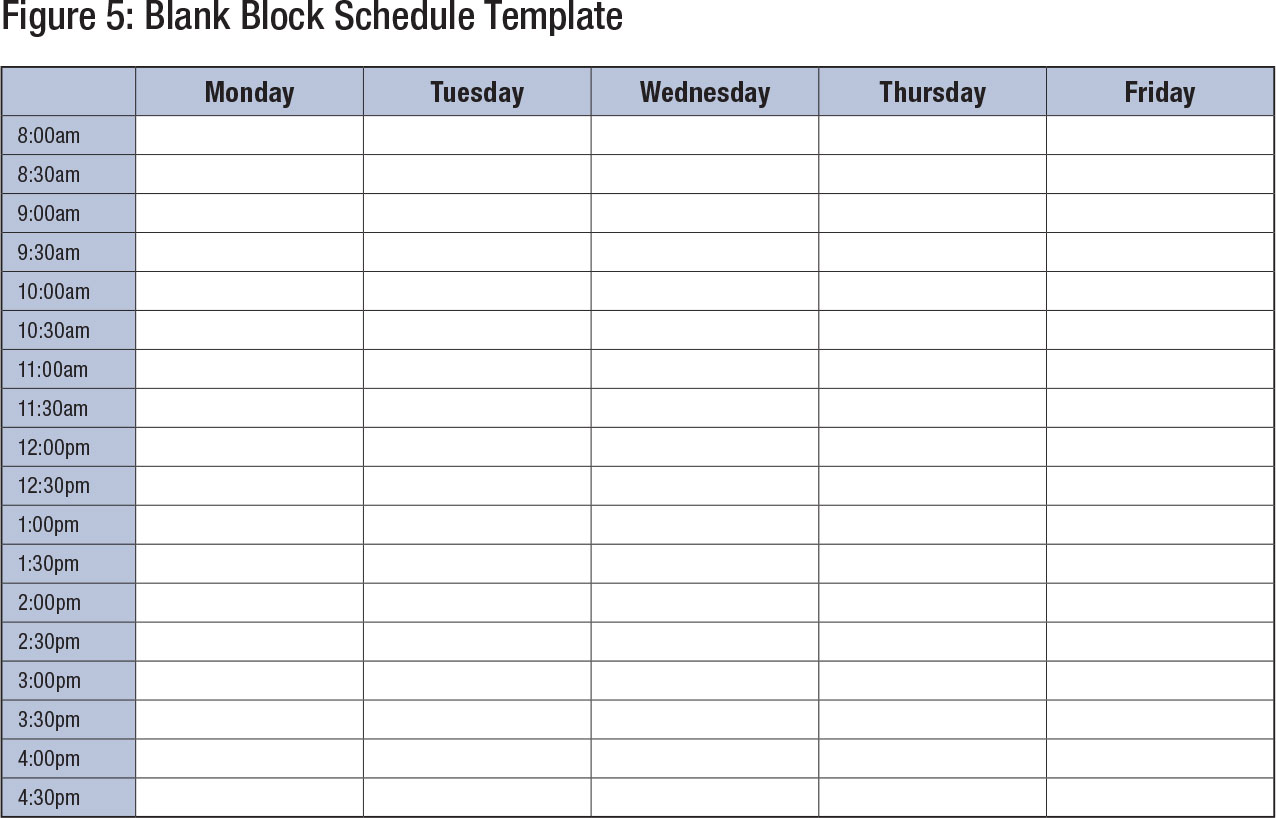
Now that all the components for the block schedule have been created, the block schedule can now be filled in with the blocks. The order in which blocks are placed should be dependent on the practice’s needs and schedule of staff. A common practice is to distribute patient filling blocks at a variety of times and days during the week to give patients as many options as possible.
Although the block schedule should ultimately reside in the practice’s Office Management System (OMS), Figure 5 represents an example of a working draft to create a variety of block schedule options for consideration. To summarize, the below bullet points are blocks that need to be added to the schedule and Figure 6 represents a completed block schedule.
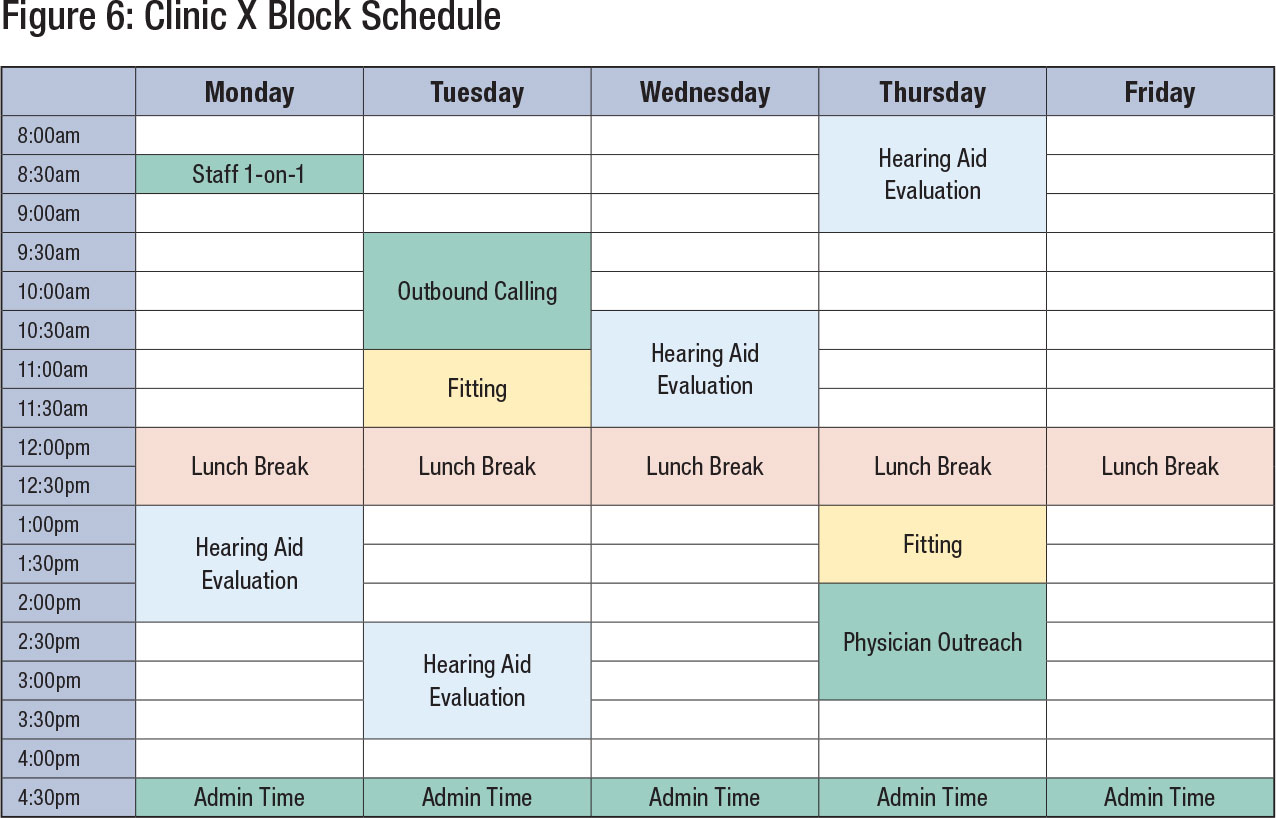
Recurring Meetings
- Weekly 5. Hour 1-on-1 meeting with Front Office Staff
- Daily Lunch Break from 12pm to 1pm
Priority Tasks
- Weekly 1.5 Hours for Physician Outreach
- Weekly 1.5 Hours for Outbound Calling
Administrative Time
- Daily .5 Hour Administrative Time for Provider
Appointment Blocks
- 4 – 1.5 Hour Hearing Aid Evaluations
- 2 – 1 Hour Fitting Appointments
- 4 - .5 Hour Follow Up Appointments
Step 4: Implementing the Block Schedule
In most instances, a practice will already have an established way of managing the schedule and many demonstrate reluctance or even resistance to the new approach. Therefore, staff must be reminded that scheduling is a three-phase process that allows the practice to use their time more efficiently.
 In Phase 1, the manager should create a sense of urgency around block scheduling, emphasizing the importance of executing this new program as seamlessly as possible. The manager can emphasize this point by assembling a strong guiding team and providing a clear vision of how block scheduling optimizes productivity by working through some financial projections when block scheduling is fully realized.
In Phase 1, the manager should create a sense of urgency around block scheduling, emphasizing the importance of executing this new program as seamlessly as possible. The manager can emphasize this point by assembling a strong guiding team and providing a clear vision of how block scheduling optimizes productivity by working through some financial projections when block scheduling is fully realized.
In Phase 2, the manager should work to reinforce the new process. If staff sees the new process as a success, they will more quickly adopt the process and be advocates of the process themselves. If the manager has successfully laid out a clear vision of how block scheduling works, it should help block scheduling gain traction and support among staff. Lastly, the manager should try to over-communicate. New processes can create uncertainty for staff, so frequent feedback from the manager on what staff are doing well and what they need to correct will be extremely beneficial during this phase.
Finally, Phase 3 is when the block scheduling process becomes established. Staff know their responsibilities and executing necessary action items goes off without a hitch. The most common challenge during this phase is complacency. It is crucial to keep the momentum of fully integrating block scheduling into the practice and correct any behaviors that embody the old practices. A best practice is regular reporting or checking in with staff, especially those who have questions about the implementation of block scheduling.
Step 5: Managing and Maintaining the Block Schedule
The most common management challenge in block scheduling is what actions to take when marketing and business development efforts fail to fill a block. A common practice for addressing this challenge is utilizing the 24- or 48-hour rule. The rule functions as an alert to the team member, in charge of the schedule that requires action, to fill an empty block that is open 24 or 48 hours prior to the actual appointment time. An example of some actions that could be taken include inquiring with patients who have a later scheduled appointment to see if they could come in earlier. Another option is to move the block to another date. This new date should be in addition to any other existing blocks. The decision as to whether the block should be 24 or 48 hours, is up to the practice and should be aligned with whichever timeframe is most effective for the practice.
Another common challenge is that blocks do not line up exactly with patients’ desired appointment times. This is a perfect example to highlight that blocks are flexible. Although blocks should not be deleted, they can be moved to accommodate a patient’s schedule so long as the time slot is not otherwise filled with other appointments.
Finally, any block-scheduled activities that have an impact on finances should be re-evaluated when budgets and targets are being set for the following year or financial timeframe. As financially based blocked schedules are established to meet financial targets, it makes sense to adjust your block schedule accordingly. For example, in a practice that does a mix of private pay and third-party contract business, it is prudent to have separate blocks for each. When open time slots are available, the more lucrative business would get first priority when filling the appointment time.
As the practice progresses through the year, monitoring progress is critical for success. There are often solutions to the challenges of block scheduling, but time is often the limiting factor that leads to failure to meet financial targets. In addition to using the 24- or 48-hour rule, progress should be reviewed on a weekly and then monthly basis. The key is identifying any deviation from financial targets as soon as possible. A reporting template should include weekly progress, year-to-date progress, as well as deviations from goals and projections, based on actual progress within the given time period.
Although a well-configured block schedule can help a practice meet its financial targets, the review of progress and accompanying key performance indicators (KPIs) will help a manager identify the types of corrective actions necessary for any deviations from targets. Any deviations from target will usually fall under one of the below scenarios.
Effective Management of the Block Schedule
There are several potential problems that can occur with a block schedule. Each of problems listed below are an opportunity for managers to provide feedback and coaching that will address the problem in a forthright and professional manner.
- Cannot Fill Time Blocks
- Weekly Review
- If a practice is struggling to fill a block in the 24- or 48-hours prior to the appointment, a best practice is to reach out to patients scheduled out in the future to see if they would like to come in earlier. This will create more time for the practice to fill a later block.
- Monthly Review
- If the practice is struggling to fill blocks on a consistent basis, the practice will want to evaluate marketing and outbound calling efforts to see if there are opportunities for generating more flow of patients into the office. It is not uncommon for a practice to have a month below target, but marketing and outbound calling efforts should be escalated until targets are being met.
- Weekly Review
- Effectiveness Ratio Drops
- Weekly Review
- If provider conversion drops below the value used for calculating the block schedule, no immediate action is required as deviations are expected.
- Monthly Review
- If the practice is struggling to convert patients on a consistent basis, the practice will want to evaluate training or professional development efforts to see if there are opportunities for the provider to help the patient overcome objections to treatment. It is not uncommon for a provider to have a month below target, but training or professional development efforts should be escalated until targets are being met.
- There is no one right answer to the decision on the ratio between private pay and third party/fitting fee patients, however this ratio should be reviewed each month.
- When working with a CPA or a financial advisor to calculate the net revenue targets, a best practice is to review one’s personal, professional, and financial goals every few months. Although it may be tempting to set an aggressive revenue goal, a packed schedule may cause personal and other professional goals to become diminished or fall by the wayside completely.
- Weekly Review
- Average Selling Price Drops
- Weekly Review
- If the Average Selling Price of Hearing Aids drop below the value used for calculating the block schedule, no immediate action is required as deviations are expected.
- Monthly Review
- If the practice is struggling to stay at or above Average Selling Price on a consistent basis, the practice will want to implement provider training or professional development efforts to see if there are opportunities for the provider to see the value in the services they provide to the patient. It is not uncommon for a provider to have a month below target, but training or professional development efforts should be escalated until targets are being met.
- Weekly Review
Leverage block scheduling to complete those tasks that are most frequently put off or never completed. By setting aside specific time slots to get those less than desirable tasks done, a practice will be less likely to set aside these tasks in lieu of more desirable or easier ones that are not a practice priority.
4. Too Many Appointments
A scenario where there is an overabundance of the desired appointment doesn’t require any corrective action but should serve as a warning to managers to be on the lookout for complacency among staff that block scheduling is ineffective or no longer needed. A block schedule may seem irrelevant, or even unnecessary, when the schedule is full, but it is imperative to remember that a block schedule will alert a practice to any adverse changes – even ones that are so gradual that a practice staff may not notice the decline in performance until is has become severe. The bottom line is that effective management of several financial objectives begins with careful and deliberate implementation of block scheduling. This is because time can never be replaced and remains our most precious resource.
Caveats to Block Scheduling
Block Scheduling is a powerful tool to help manage time, but it is not recommended for every type of appointment or activity. As block scheduling requires ongoing monitoring and maintenance, it is a best practice to save block scheduling for critical business tasks. Minimizing tasks for block scheduling also reinforces the level of importance the block schedule and associated monitoring and maintenance tasks are to the business. A few of the tasks not recommended for block scheduling include:
- Repairs
- Clean & Checks
- Annual Hearing Tests
- Warranty Checks
- Diagnostic Test
Time should be set aside each week for walk-in patients or the provision of virtual care.
The primary benefit of block scheduling is to help a practice reach financial goals and more effectively manage time. Any task that is critical to a business’ success is a candidate for block scheduling. The following tasks should be considered for block scheduling:
- Recurring Meetings (Team Member 1-on-1’s, Staff Meetings)
- Priority Tasks (Outbound Calling, Patient Follow Up Calls)
- Administrative Hours (report writing, billing)
- Hearing Aid Evaluations
- Fittings
- Follow-up appointments
- Annual hearing checks
Any task, when done in excess, can detract from the success of the business. In an audiology practice, an appointment type that has a low margin or causes the practice to lose money, could be considered for reverse block scheduling. In our experience, adoption is the most common challenge associated with block scheduling. A best practice for addressing this challenge is through a robust implementation that includes a strong guiding team, a clearly articulated vision, and a sense of urgency. These elements are reinforced through consistent and clear communication about expectations and results. A team should also be empowered to act when the plan needs to be calibrated to meet targets — a process that starts with clear-eyed effective management leading a productive staff. ■
Zach Malone and Ron Patton are operations managers for Audigy.
