
AI-Driven Solutions: Revolutionizing the Way We Deliver Hearing Healthcare
Donald W. Nielsen, PhD
- Portions of this article originally appeared in Nielsen, D., W., 2024, The Intelligence Revolution in Hearing Healthcare Delivery, A Fuel Medical Group publication, Available at https://fuelmedical.com/wp-content/uploads/2024/05/fm_march2024_intelligence_revolution_paper_v1-1.pdf
Get ready to discover the astonishing reinvention of hearing healthcare. Generative artificial intelligence (GenAI) is the leading platform for revolutionizing healthcare and addressing numerous challenges. It is restructuring and modernizing the provision of healthcare.
GenAI-enabled hearing healthcare delivery will transform and enhance hearing healthcare (HHC) provision by utilizing AI to assign providers most efficiently and effectively and even create more providers. Importantly, it promises to significantly improve access and affordability, a key concern in the healthcare industry, fostering a sense of hope and optimism for the future of HHC.
HEARING HEALTH CARE’S PATIENT POPULATIONS
To truly grasp GenAI’s transformative power in providing HHC, we must first acknowledge the diversity of our patient base and their unique needs. This patient diversity, coupled with the assortment of needs, is not a challenge but a driving force behind the redefinition of HHC providers and the transformation of their roles. Here is where we stand today.
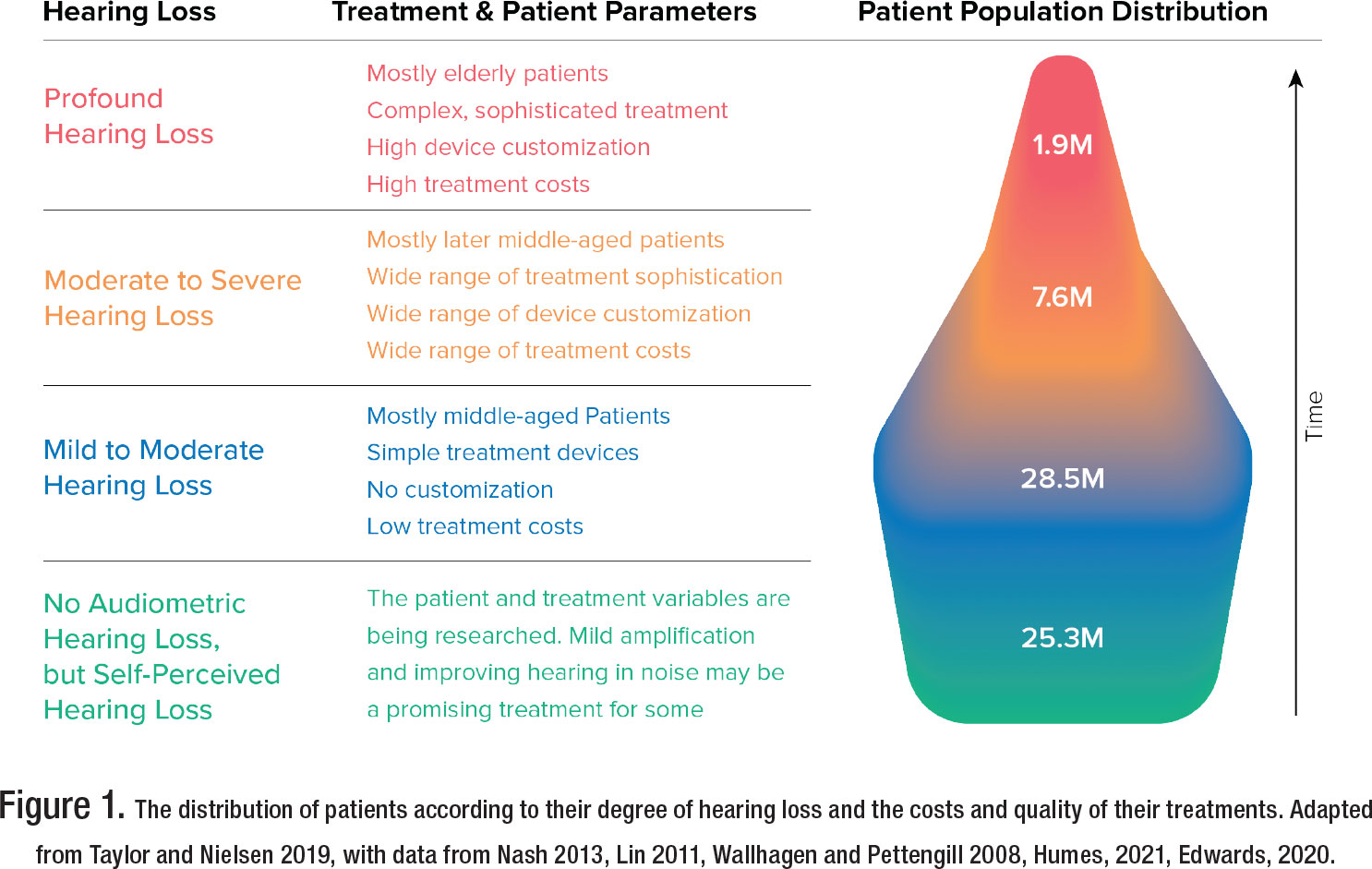
Figure 1 illustrates that 75% of patients with measurable hearing loss have mild or moderate losses, while only 5% have profound hearing loss. There are overwhelming differences in the healthcare needs of these patient groups.
Much hearing loss is chronic, and as time passes, it gets more severe, so treatments and providers must evolve to accommodate those changes. Grouped by the severity of hearing loss, the illustration clarifies the significant differences in costs, treatments, and expertise needed to serve each group.
The main point is that audiology is undergoing a significant change because we can now utilize GenAI to effectively serve different patient groups by aligning their specific requirements with appropriate care, resulting in lower expenses and improved accessibility.
THE PIVOTAL THEME: MATCH THE PROVIDER TO THE PATIENT’S NEEDS
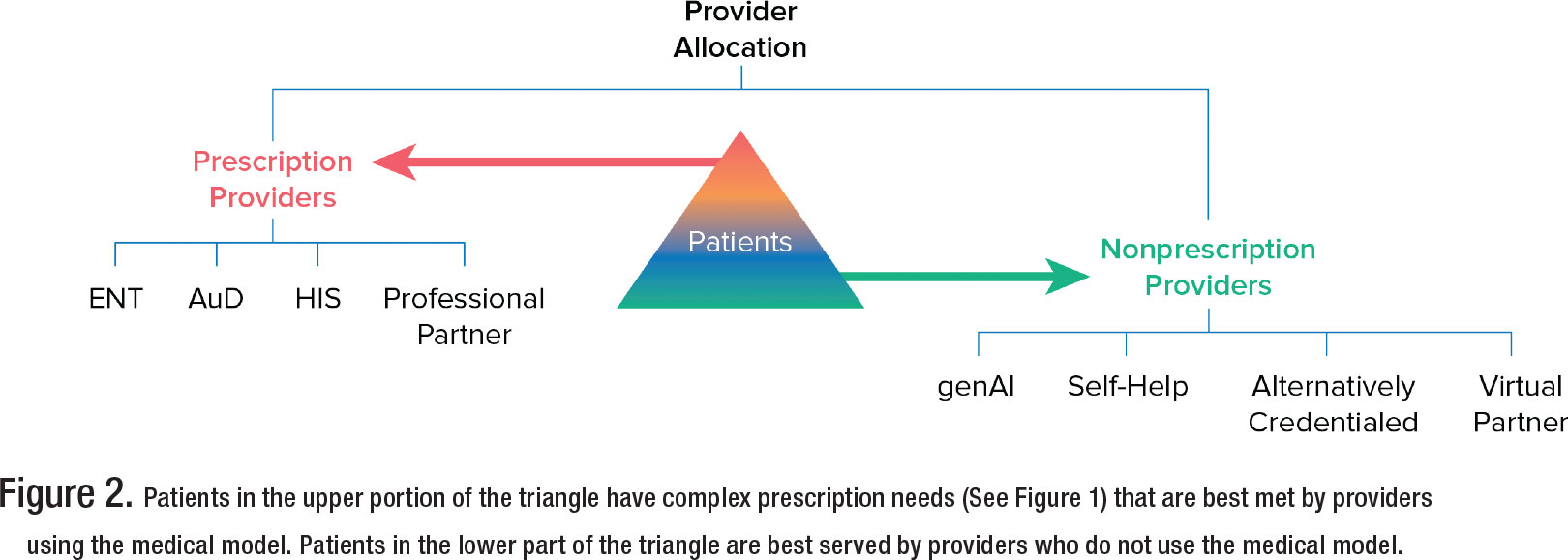
Figure 2 illustrates that we must split the diverse patient base in Figure 1 into those requiring medical model care (prescription providers) and those who will do well with nonmedical model care (nonprescription providers). This triaging matches the patient’s needs to the appropriate provider and allows us to assign providers most efficiently and effectively while improving access and affordability. Let’s take a closer look.
AI’S ROLE IN FACILITATING THE PATIENT/PROVIDER MATCH
Figure 1 shows HHC patients distributed according to their hearing loss. However, people don’t know where they are in this population distribution or which providers they should see. They require guidance to match their needs with the right provider. AI’s enormous contribution to HHC is its ability to facilitate that match and even create new providers.
AI’S ROLE IN MATCHING HHC PATIENTS AND PROVIDERS VIA PRIMARY CARE PROVIDERS (PCPS)
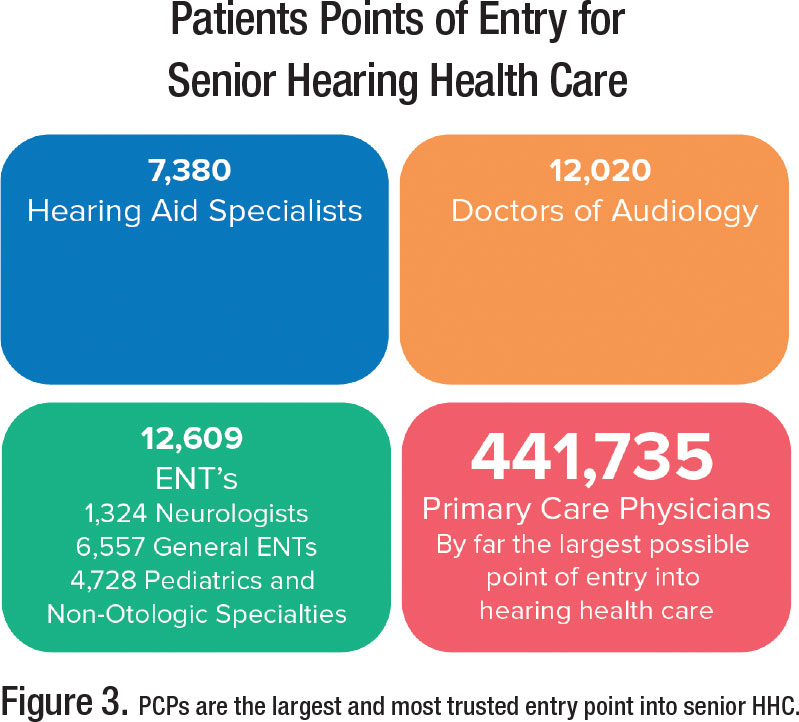 Why PCPs matter: PCPs play crucial roles in HHC. PCPs are often the patient’s initial interaction point. They are responsible for identifying hearing loss in Medicare’s annual wellness exam. HHC patients are twice as likely to seek treatments, ranging from OTCs and hearing aids to implant surgeries, if a PCP recommends them.
Why PCPs matter: PCPs play crucial roles in HHC. PCPs are often the patient’s initial interaction point. They are responsible for identifying hearing loss in Medicare’s annual wellness exam. HHC patients are twice as likely to seek treatments, ranging from OTCs and hearing aids to implant surgeries, if a PCP recommends them.
The problem: HHC has not been a top priority for PCPs. Only 12% of PCPs refer patients to hearing care, and many are confused or anxious about identifying the hearing health path their patients should follow. As a result, hearing issues can go undiagnosed and untreated or not seen by the optimum provider.
The AI solution: We can embed HHC-based AI in primary care annual wellness intake forms to identify more people with hearing issues, diagnose them correctly, and guide them to the proper treatment device and provider.
An example: HCRpath, created by Sara Sable-Antry (www.hcrpath.com), provides an example of how AI embedded in a PCP’s intake forms provides a solution that benefits patients, PCPs, audiologists, and ENTs. Here is how it works:
- HCRpath AI embedded in Medicare wellness exam intake forms identifies hearing loss and if the patient needs a medical exam to diagnose their hearing issues.
- HCRpath considers a broad range of hearing devices, from simple nonmedical amplification devices to sophisticated medical devices, and matches the patient to the appropriate device suggestions based on its analysis.
- HCRpath considers several providers and suggests the most appropriate providers that the PCP could recommend to the patient.
In addition, HCRpath has several additional advantages, including audiologists benefiting from more referrals for those patients genuinely concerned about hearing difficulties and ready to receive treatment. See www.hcrpath.com for more details.
This example demonstrates that AI embedded in the Medicare intake forms does not replace audiologists. Instead, AI, as the PCP’s co-provider, makes informed decisions that guide only appropriate patients to their optimum providers, maximizing the providers’ time and services. In the future, this approach can benefit significantly from including genomic information and other personal information in the patient’s database and its integration into the intake form analysis.
To modernize the provision of HHC, a strong partnership between HHC providers and PCPs is necessary. AI can facilitate and strengthen that relationship. Audiology’s involvement adds credibility and sophistication. We must work toward integrating AI-enabled HHC in the PCPs domain. Audiologists will gain from working with PCPs and their AI systems to be the clinicians or clinics the AI recommends.
Let’s turn to AI’s role in solving other HHC problems centered on matching the patient and provider.
AI’S MODIFICATION OF HHC DELIVERY
The recent blossoming of GenAI and the concurrent proliferation of nonprescription hearing treatments have reshaped how audiologists can serve the lower portion of the patient triangle who benefit from nonprescription providers. These emerging provider types include self-help and virtual partners, both of which benefit from GenAI empowerment.
A NEW GENERATION OF AI-ENABLED PROVIDERS ARE AUDIOLOGY EXTENDERS
Self-Help: Patients as Partners: A limitation to increasing patient information access and encouraging patients to investigate their problems is that we have thought of patients as passively waiting and then engaging a doctor when treatment is necessary. However, increasing offerings improved by GenAI let patients identify and triage medical issues and care for them independently, only bringing in a doctor when required. Meanwhile, medical devices customized for self-help are moving from the doctor’s office to the home. Even cochlear implant recipients can self-test at home to monitor implant performance with smartphones or tablets (Wasmann et al., 2023).
Because of these changes and the mismatch of provider supply and demand, individuals are becoming long-term stewards of their hearing health. Viewing patients as medical self-health stewards makes them partners in the medical process. It acknowledges that there may be no other person or institution with a corresponding level of information, incentive, or influence as the individual. It does not undermine the role of the medical community and its institutions. It makes it more efficient (Hartenstein and Latkovic, 2022).
Virtual Providers: GenAI allows us to provide accessible, competent virtual providers instead of one-on-one in-person medical care when patients need constant or repetitive instructions. The AI that empowers virtual providers and self-help assistance is the same. We call it telepresence. Let’s take a deeper dive into its operation and use.
AI ENHANCEMENT OF TELEPRESENCE
Telepresence — These technologies allow people to feel as if they are physically present with someone whom technology represents digitally. In prescription HHC, telepresence can be an essential part of digital therapeutics (DTx) to treat and manage diseases. DTx are patient-facing software applications that help patients treat, prevent, or manage a disease and have a proven clinical benefit. Given the widespread use of cell phones and computers, telepresence is rapidly evolving to strengthen health care and increase affordability and accessibility.
Previous virtual technologies, like Internet chat blogs, were not lifelike or personal—questioning and answering required laboriously written interactions with long delays, frustrating misspellings, and mistaken interpretations. Notably, the elderly find them challenging and unnatural.
Videos are an improvement over text-based chatbots; however, if you have assembled furniture while watching a YouTube video, you understand the limitations of the video instructional model. Self-help videos give limited instructions, lack interactions, and are often problematic.
AMIE is a chatbot created before GPT-4o to provide medical advice to patients. It was compared to human doctors to assess its ability to show empathy and engage in conversations. AIME performed better than doctors in 24 out of 26 aspects of conversation quality, offering patients an equal or higher level of empathy and support as human physicians (Haseltine, W., 2024).
Virtual providers using GenAI, like AIME, can learn, converse, and problem-solve like humans. Still, with the advent of GPT-4o, they can do better because GPT-4o is natively multimodal, which means it can “see,” “hear,” and “speak” in an integrated way with almost no delays. It can blend all of these modes together. It can see what you are doing, react to it, respond to interruptions, use realistic voice tones, and create images. Virtual providers can react like humans and influence patients as humans do (Mollick, E. 2024). GPT-4o is free. Experiment with it to discover its many attributes and imagine its use with 3D virtual providers. Virtual providers can exceed routine human communication by using captioning, clear speech, synced in—focus, and accurate lip movements. They have quickly evolved to be competent coworkers.
Contrary to popular belief, AI can express emotions by reacting to the feelings of others. GenAI-based systems can determine a patient’s emotional state by analyzing speech patterns and other cues, such as facial expressions and physiological measures. These systems can help inform a virtual provider in real time if the patient is or is not engaged and what material is resonating. The virtual presenter could slow down, show more empathy, or make other changes. Patients will develop relationships with virtual providers as they do with friendly front office staff and human providers.
GenAI facilitates the development of new care delivery capabilities that fundamentally change how HHC teams spend their most valuable resource: time. Now, we can provide patients with needed information 24/7 from a virtual person who analyzes vast amounts of patient data, answers any verbal or written questions, and presents a pleasant, empathetic personality. As the virtual partner acquires more knowledge, it improves with use.
GENAI’s INFLUENCE ON OTC DELIVERY AND ACCEPTANCE
By allowing patients to feel as if they are physically present with someone whom technology represents digitally, telepresence can transform over-the-counter (OTC) hearing aid adoption. The FDA promoted OTC hearing aids to provide high-quality hearing aids that people with mild to moderate hearing loss could buy online or at local pharmacies and bigbox stores. However, acquiring hearing aids over the counter can still feel challenging. Not everyone with hearing loss is comfortable with online sales or do-it-yourself adjustments via apps. ASHA’s OTC Hearing Aid Survey, 2023, found that only 24% of those patients who were at least somewhat confident an OTC device could assist them were satisfied they could choose the correct device. They need help.
AI-enabled platforms could be the key to adopting more excellent value-based care options. Consider how helpful interactive dialog with a quality virtual provider could be in informing patients about OTC devices. Patients could discuss if the devices are appropriate treatments for their hearing issues. If so, they can also get suggestions about which OTC device to purchase and how to unbox, fit, and maintain it. This system would introduce patients to HHC in a less expensive, more accessible, more prosperous, and more rewarding way than it currently does.
Perhaps the ultimate telepresence innovation is Google’s Project Starline, which, without 3D glasses, provides the patient with a life-sized 3D image across the table from them: www.youtube.com/ watch?v=obuyCkotJ_s. No more flat, boring screens! The image is so lifelike that people try to reach out to each other to shake hands or fist bump. That 3D image could be a virtual representation of their personal physician or audiologist equipped with precision medicine knowledge, sensitive to the patient’s emotions, and available 24/7 for consultation.
The more true-to-life experience of 3D and holographic medicine is already with us. The University of Central Florida, see: healthprofessions. ucf .edu/rehabi l it at ion-innovat ioncenter/# contact, uses holograms to train students and educate patients.
Virtual reality headsets are like having a computer strapped to your face. In time, these headsets will be inexpensive enough for healthcare systems and insurers to provide them so their patients can consult with a 3D virtual healthcare provider 24/7, creating a massive transformation in healthcare. AI-powered virtual health care has the potential to be both convenient and cost-effective. Patients no longer need to schedule appointments, travel to a healthcare provider, or wait for an in-person, one-on-one meeting with their provider.
AI’S EFFECTS ON PRESCRIPTION HHC
In-Office AI-Enabled Audiology Extenders: While selfhelp and remote virtual providers will improve HHC access, in-office AI-enabled providers like AMTAS Pro will also be needed to accompany prescription care.
AMTAS Pro: This is made by GSI and provides an Automated Method for Testing Auditory Sensitivity. It is an in-office patient-directed hearing assessment tool that uses AI to obtain diagnostic or screening audiometry. Imagine the benefits of freeing up the time to perform complete diagnostic testing.
AMTAS Pro is self-paced, so patients may proceed at a rate that is comfortable for them. A complete diagnostic evaluation will typically take 15–20 minutes for the patient to complete independently, which provides more time for the audiologists to attend to other patients.
Whoever dominates the interactive telepresence approach to OTCs will capture the mild hearing loss market and be the provider of choice for more weighty hearing issues as the patient’s hearing deteriorates with age.
Audiology extenders are essential in freeing audiologists from routine testing tasks to reallocate their time to the most complex patients who can only succeed with audiologists participating in their HHC. In-office AI-enabled audiology extenders fulfill this role while reducing costs.
CONCLUSIONS
Believing that tomorrow will be similar to today is a deepseated human bias, as it is typically true. However, not at this moment!
The fields of GenAI, genomics, precision medicine, and computer-driven big data analysis/systems are all flourishing and advancing simultaneously. These combinations of innovation and technology offer HHC private practice providers multiple new, better, and more competitive options for the future.
By directing the appropriate patients to new GenAI-equipped channels to diagnose and treat their nonprescription HHC needs, GenAI will streamline patient triage so only those needing qualified prescription-capable providers will see physicians and audiologists. This liberation of prescription providers will result in more patients with prescription needs being appropriately seen and treated, significantly improving HHC.
GenAI-driven precision medicine also increases the power and scope of prescription providers by allowing them to analyze enormous datasets, glean hitherto unavailable relevant information, and research that information to make patient-personalized diagnostic and treatment decisions. Because of GenAI, precision medicine can revolutionize the provision and delivery of prescription HHC. For an introduction to precision medicine, see Nielsen (2024). I explain it in more detail in an upcoming new Fuel Medical Group white paper, “Genomics and Precision Medicine: The Astonishing Reinvention of Hearing Healthcare.”
To achieve growth and success, audiology must leave behind outdated practices from the 1900s and embrace new delivery methods that take advantage of rapidly evolving opportunities to effectively treat more patients, deliver improved care, and provide hope, optimism, and a viable strategy for the future. ■
References
- ASHA’s OTC Hearing Aid Survey, 2023, Comprehensive polling report [PDF]. https://www.asha.org/siteassets/press-room/asha-otchearing- aid-survey-report-2023.pdf
- Edwards B., (2020). Emerging Technologies, Market Segments, and MarkeTrak 10 Insights in Hearing Health, Seminars in Hearing Vol. 41, NO1, pp. 37–54.
- Hartenstein, L., Latkovic, T. (2022) The Secret to Great Health? Escaping the healthcare matrix, McKinsey Health Institute, December 2022. Available at: https://www.mckinsey.com/mhi/ our-insights/the-secret-to-great-health-escaping-the-healthcarematrix? cid=eml-web
- Haseltine, W., (2024), Medical Artificial Intelligence: A New Frontier in Precision Medicine, Inside Precision Medicine, February 2024, p46-49. https://www.insideprecisionmedicine. com/topics/informatics/medical-artificial-intelligence-a-newfrontier- in-precision-medicine/.
- Humes, L. E., (2021). An Approach to Self-Assessed Auditory Wellness in Older Adults, Ear & Hearing, Vol. 42, NO, 745-761. Lin, F.R., Niparko, J.K., Ferrucci, L., (2011). Hearing loss prevalence in the United States, Arch Intern Med: 171(20):1851-1852. Mollick, E. (2024) What Open AI did. , oneusefulthing@substack. com, May 14.
- Nash, S.D., Cruickshanks, K>J>, Huang, G.H. et al. 2013, Unmet hearing health care needs: the Beaver Dam offspring study. Am J Public Health;103(6):1134–1139.
- Nielsen, D., W., 2024, The Intelligence Revolution in Hearing Healthcare Delivery, A Fuel Medical Group publication, Available at https://fuelmedical.com/wp-content/uploads/2024/05/fm_ march2024_intelligence_revolution_paper_v1-1.pdf.
- Taylor, B. S., Nielsen, D.W., (2019). Entrepreneurial Audiology: Sales and Marketing Strategies in the Consumer-Driven Health Care Era, in Audiology Practice Management, 3rd Edition, Edited by Brian Taylor, Thieme Publishers.
- Wallhagen, M.I., Pettengill, E., (2008). Hearing impairment: significant but underassessed in primary care settings; J Gerontol Nurs: 34(2):36-42.
- Wasmann, J-W., A., Huinck, W., J. and Lanting, C., P., (2023), Remote Cochlear Implant Assessments: Validity and Stability in Self-administered Smartphone-based testing, Ear and Hearing, Vol. 45, NO 1, 239-249. Wolters Kluwer Health, Inc.
Donald W. Nielsen, PhD, is a senior consultant for the Fuel Medical Group in Camas, WA. Dr. Nielsen can be reached at
