
Differentiation Through a 21st Century Audiologic Evaluation Model
There is a great deal of talk about the value of provider driven, audiologic evaluation and its superiority to evaluation delivered by other means (i.e. computerized, self-assessment, or online) or by other providers (i.e. hearing aid dispensers or technicians). There is no doubt that, when delivered to the research evidence, audiologic evaluation performed by an audiologist is the gold standard of hearing care. Study after study illustrates this.
The issues I continue to have and try to bring to the forefront is: Does every patient, in every situation, require inconsistently delivered, gold standard evaluation to treat their hearing loss and communication difficulties? If yes, are the majority of audiologists in the US consistently providing this “gold standard” care? The data still does not illustrate that a majority of audiologists do.
To get to the heart of this, let’s break down the most common audiologic evaluations: the audiogram.
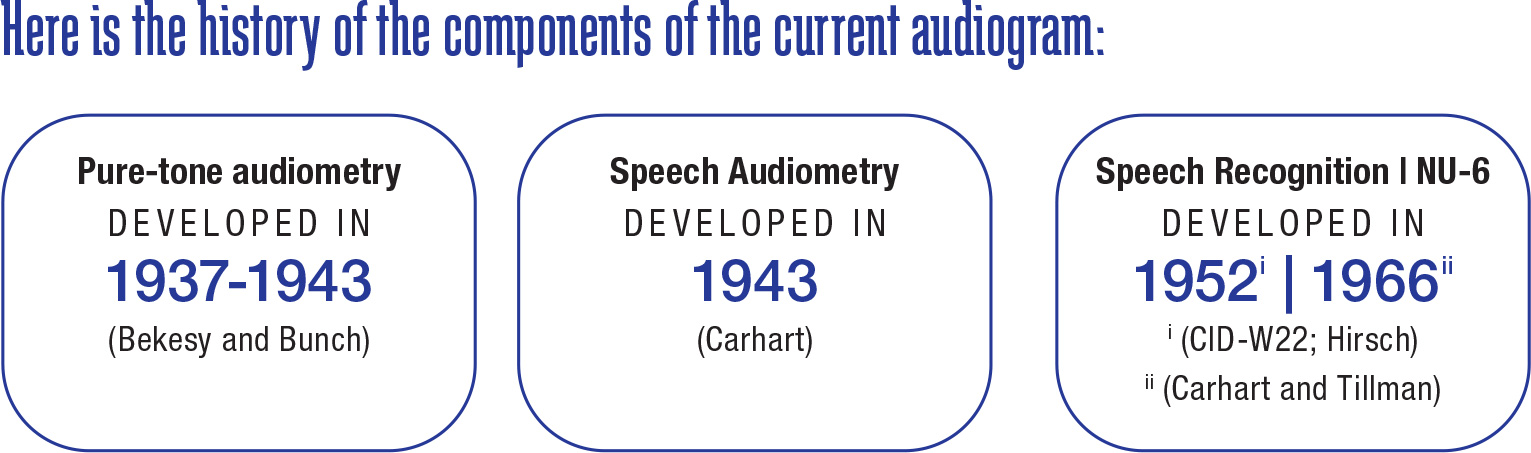
Audiologists are almost entirely using these evaluation techniques, from over a half century ago, to evaluate hearing loss and fit today’s hearing technology. My question is: Why? Why have we not evolved our model?
As a profession, we voice frustration about disruptive competitors and scope creep by less trained hearing care professionals yet still do not combat this by doing things differently. We don't provide and document the minimally medically necessary services to diagnose the patient’s otologic condition and/or hearing loss and create and implement a comprehensive treatment and rehabilitation plan. For example, people talk about the research outcomes of ACHIEVE yet avoid the standard of care that was provided in the project to reach those outcomes. It is like we all completely ignored the method section.
Unless required by your state hearing aid dispensing law or a health plan payer policy, audiologists need to begin to ask themselves: What does the patient in front of me right now need to determine their otologic and audiologic function and status and create a comprehensive treatment plan that meets their individual hearing and communication needs? Why I am I doing what I am doing with and for this patient?
In my opinion, the minimum test battery for a new adult patient, again unless dictated by the state law or payer policies, should include:
- A standardized inventory/questionnaire of communication difficulties, such as the COSI, HHI, IOI, or SAC.
- Pure-tone, air conduction audiometry.
- Pure-tone, bone conduction audiometry or a Consumer Ear Risk Disease Assessment.
- Speech in noise testing.
- Patient/family interview regarding the patient’s lifestyle, cosmetic desires, the psychological, medical, educational, emotional, social, and/or vocational impact of chief complaint and any financial limitations.
The rest of the common test battery not listed above should be provided as medically necessary for the specific, individual patient. ■
