Promoting Hearing Care Literacy to the Medical Community Through the Virtuous Cycle of Patient Engagement
Brian Taylor, Au.D. and Bob Tysoe
A growing body of evidence shows that individuals with the knowledge, skills, and confidence to become actively engaged in their health care are more likely to experience better health-related outcomes (Domecq, et al 2014). The term patient engagement is used to describe this process. There are several facets of patient engagement, including motivation and self-confidence. Moreover, specific skills such as the individual’s reading level and listening ability, which form the core of health literacy, influence patient engagement. While an individual’s motivation and self-confidence to engage in health self-management often are not measured as part of health literacy, they are included in measures of patient activation. The bottom line is that individuals who are not engaged in their own healthcare, as well as the decision-making process surrounding it, are much more likely to have poor health literacy. Therefore, it is essential for audiologists to identify help-seeking individuals who are at risk for poor health literacy and offer solutions that are aligned with these lower health literacy levels.
Of course, patient engagement and health literacy are important factors in the clinic when working directly with patients. However, given that most adults with hearing loss fail to seek help from an audiologist, it is imperative for those professionals to find ways to bolster the hearing health literacy and patient engagement of those individuals at risk for hearing loss in the medical arena – places where older adults are likely to be receiving regular care from a primary care physician. The purpose of this article is to provide audiologists with a systematic plan for how they can work directly with the medical community to strengthen patient engagement in those at risk for hearing loss. The main idea being that patients who experience a higher level of engagement with their physician are more likely to engage in services delivered by an audiologist.
Scope of the Challenge
 It is well known that age-related hearing loss is both undertreated and inadequately treated. Current estimates suggest that about 20% of adults with hearing loss in the United States wear hearing aids (Lin et al, 2011). Further, while a higher percentage of individuals with severe hearing loss wear hearing aids, less than 10% of them who meet the candidacy criteria for cochlear implants have undergone cochlear implant surgery (Sorkin & Buchman, 2016) – an intervention that is usually more effective than traditional hearing aids for the proper candidate (Boisvert, et al 2020). Thus, it is fair to conclude that many adults with severe hearing loss are inadequately treated, while those with milder hearing loss are under-treated.
It is well known that age-related hearing loss is both undertreated and inadequately treated. Current estimates suggest that about 20% of adults with hearing loss in the United States wear hearing aids (Lin et al, 2011). Further, while a higher percentage of individuals with severe hearing loss wear hearing aids, less than 10% of them who meet the candidacy criteria for cochlear implants have undergone cochlear implant surgery (Sorkin & Buchman, 2016) – an intervention that is usually more effective than traditional hearing aids for the proper candidate (Boisvert, et al 2020). Thus, it is fair to conclude that many adults with severe hearing loss are inadequately treated, while those with milder hearing loss are under-treated.
What is patient engagement?
The essence of patient engagement is providers and patients working together to improve health. A patient’s engagement in health care contributes to improved outcomes, Information technologies such as social media, user-friendly websites and educational materials available on-demand can support engagement. Patients want to be engaged in their healthcare decision-making process, and those who are engaged as decision-makers in their care tend to be healthier and have better outcomes.
It is widely believed there are several factors associated with under-treatment and inadequate treatment of adult onset hearing loss. One, access to providers who specialize in treatment of hearing loss, especially surgeons who perform cochlear implant surgery, is a problem in many rural parts of the country. Long travel times and even long wait times to see the surgeon are significant barriers. Two, there are misconceptions about device candidacy and the risks associated with them. Many persons with severe hearing loss (and even some audiologists) believe that cochlear implants are reserved for the most profound hearing loss. Three, there is poor awareness among the general population about the consequences of untreated hearing loss, which can be harmful. In general, the public still largely thinks hearing loss is a completely benign consequence of the aging process.
A recent study underscores the three points listed above: the general population has a poor understanding of what constitutes normal hearing as well as the assortment of viable treatment options available to them, including over-the-counter (OTC) hearing aids, prescription hearing aids and cochlear implants. Carlson et al (2022) surveyed 1250 adults between the ages of 50 and 80 years old. Only 9% of the respondents were able to correctly identify what constitutes a “normal” range for hearing. The authors compared the respondent’s knowledge of hearing loss to other common chronic conditions and found that 93% were able to identify the “normal” range for vision, 85% for blood pressure and 52% for high cholesterol.
Further, when respondents were asked to rank order the importance of addressing hearing loss within the context of ten other conditions, hearing loss was ranked near the bottom of the list. Perhaps the most eye-opening finding in their survey was that respondents were twice as likely to routinely bring their pet to a veterinarian than have their hearing evaluated.
 All told, this survey indicates that most middle aged and older adults, segments of the population most likely to have hearing loss, are unaware of its consequences, the comorbidities associated with it, how and where to have their hearing assessed, and the wide range of current treatment options that could both improve communication and quality of life. Clearly, the results of this survey serve as a call to action: hearing care professionals of all stripes must improve the hearing health literacy of the general adult population.
All told, this survey indicates that most middle aged and older adults, segments of the population most likely to have hearing loss, are unaware of its consequences, the comorbidities associated with it, how and where to have their hearing assessed, and the wide range of current treatment options that could both improve communication and quality of life. Clearly, the results of this survey serve as a call to action: hearing care professionals of all stripes must improve the hearing health literacy of the general adult population.
Hearing Health Literacy in the Medical Community
Perhaps more disconcerting, the problem of poor hearing health literacy is not confined only to the general public, as demonstrated in another recent survey, conducted by the same authors. Sydlowski et al (2022) surveyed 205 primary care physicians and 201 nurse practitioners or physician assistants. Their results yielded these four conclusions.
- Less than half of survey respondents (36%) reported they recommended annual hearing tests for patients, while assessment of blood pressure cholesterol, body mass index and blood glucose levels were recommended at least annually by more than 80% of the respondents.
- While upwards of 90% of survey respondents know the “normal” metrics for blood pressure, cholesterol, body mass index, blood glucose and vision, but only 57% of the respondents could define the standard definition of normal hearing. And an even lower number (24%) had familiarity with the concept of “20/20 hearing.” (The Hearing 20/20 campaign is a new public health initiative to adopt 20/20 as a common metric for normal hearing. It was launched in the fall of 2020.)
- Although most of the survey respondents stated that hearing is important to overall health, leads to social isolation, and negatively affects quality of life, a paltry 40% of the respondents believed that hearing loss is treatable. Smaller numbers (20%) believed hearing loss is a normal part of aging, and fewer still (17%) realize that hearing loss is preventable.
- Relative to other important medical conditions to manage, hearing loss came in dead last. Specifically, survey respondents were given a list of ten other important conditions, including heart disease, COPD, arthritis, cancer, asthma, obesity and others, hearing loss was tied for last by the respondents. Although many of the conditions on this life are considered life threatening when not properly diagnosed and treated, a mere 46% of respondents reported that they discussed hearing test results with patients. Given that hearing loss ranked last on the list, and that it was discussed with patients by less than half of the respondents, suggests hearing loss and its consequences are not a high priority for most providers.

The gap between the impact of hearing loss on daily living and whether medical professionals believe it can be treated and prevented is illustrated in Table 1. The survey results appear to suggest that most medical professionals are well versed in the consequences of age-related hearing loss but many lack knowledge and insight on prevention and treatment strategies. Notice in Table 1 that two-thirds or more of respondents stated that hearing loss impacts quality of life (84%), leads to social isolation (78%), impacts safety (76%) and is important to overall health (67%). In contrast, 40% or fewer reported that hearing loss is treatable, a normal part of aging and preventable. This gap is an opportunity for audiologists to raise awareness and educate the medical community about prevention and treatment strategies for age-related hearing loss.
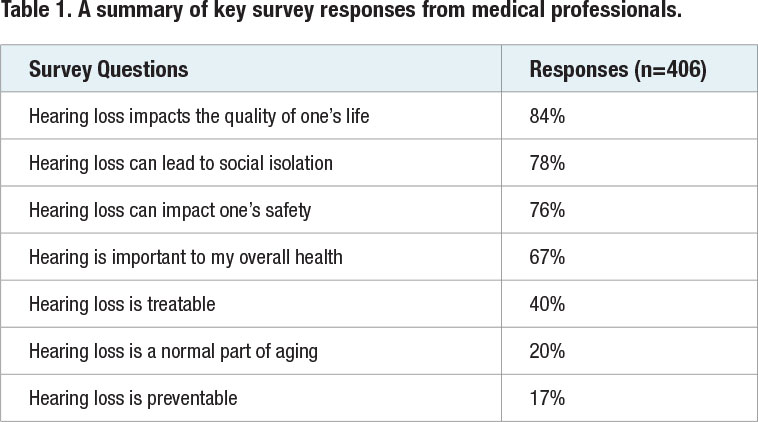

 Let’s more carefully examine the three survey questions in which the minority of respondents cited low aptitude and offer a course of action that reverses this trend.
Let’s more carefully examine the three survey questions in which the minority of respondents cited low aptitude and offer a course of action that reverses this trend.
- 17% believe hearing loss is preventable
- 20% believe hearing loss is a normal part of aging
- 40% believe hearing loss is treatable
For each of these topics, how can audiologists turn the tide and improve hearing health literacy among medical professionals? It’s starts with the ability to execute these four tactics.
1. Create an engaging format to deliver educational materials
We live in a world where people digest information in short bits. Whether that information is delivered in print, via video or through social media, the content must be brief and visually attractive. Audiologists are encouraged to share their knowledge published research that demonstrates hearing loss is preventable, a normal part of aging and treatable.
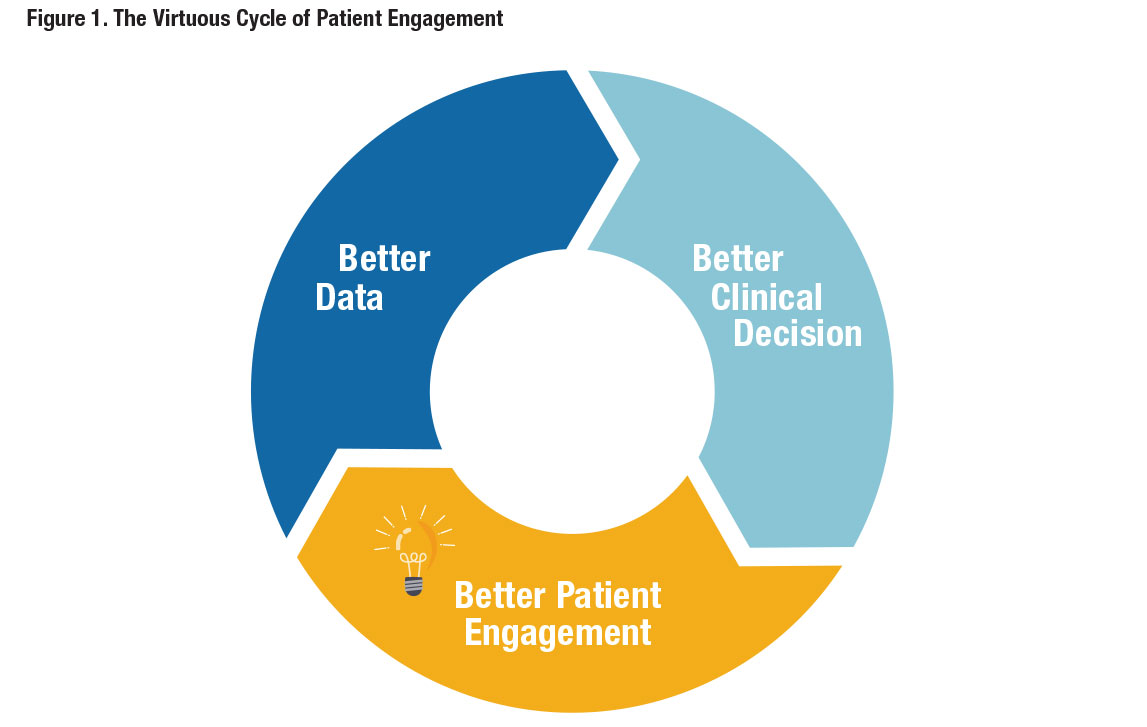
2. Feed the Virtuous Cycle of Patient Engagement with Timely and Relevant Content
Physicians and other medical professionals are trained to use research as part of their clinical decision-making process. Known as evidence-based practice, this process can be viewed as a virtuous cycle, like the one shown in Figure 1. The process starts with data, gathered from well-designed clinical studies. This data yields better clinical decisions which yields better patient engagement, which in turn, leads to the creation of better data. The audiologist’s ability to provide evidence-based content in a manner that is succinct, and to-the-point is a proven approach to feeding the virtuous cycle with better data.
3. Communicate consistently
Once you’ve decided upon an engaging format and created content that feeds the virtuous cycle of patient engagement, the next step is to deliver the content consistently. This means establishing a rhythm in which content is delivered the same time each week or each month. For example, identify physician practices in your community or geographic footprint and correspond with them using a monthly electronic newsletter that educates on the prevention, identification, and treatment of hearing loss.
4. Provide solutions that reduce communications barriers during in-person appointments
Given the prevalence of hearing loss among the aging population, there are several points of interaction older adults have with medical practices that can benefit from the insights of audiologists. Persons with hearing loss can experience many barriers when using a physician’s services, including when booking appointments over the phone, in-person interactions with the receptionist upon check-in, and while conversing with medical staff during appointments. Audiologists can provide an array of services that help the entire medical staff communicate more effectively with persons with hearing loss. These services include providing tips for talking on the phone, improving the room acoustics for better listening, and the provision of high quality non-custom amplifiers that can be used on an as needed basis.
A Two-Pronged Strategy
The results of the two surveys mentioned in this article suggest that both the general public and the medical community demonstrate significant gaps in their knowledge of hearing loss and its prevention, identification, and treatment. It’s up to audiologists to close these gaps by reducing apathy and raising awareness of the consequences of untreated hearing loss – on daily communication and interaction with medical staff during all-important wellness visits and overall quality of life. We propose a two-pronged strategy using the four tactics outlined above. This starts by educating the general public in your community at every available opportunity. Providing the general public better data about hearing loss and its consequences and possible treatments is likely to yield among this group, better, more proactive decisions about their hearing care, which in turn, yields better patient engagement and feeds the virtuous cycle with better data about outcomes that can be shared with the public.
For the medical community, following these four tactics will translate into better patient engagement that can close the gap on hearing health literacy. After all, more engaged medical professionals are likely to produce more engaged patients. This translates into more persons with hearing loss taking an active role in their care, improving the quality of life of people as they age. ■
References
- Boisvert, I., Reis, M., Au, A., Cowan, R., & Dowell, R. C. (2020). Cochlear implantation outcomes in adults: A scoping review. PloS one, 15(5), e0232421.
- Carlson, M. L., Nassiri, A. M., Marinelli, J. P., Lohse, C. M., Sydlowski, S. A., & Hearing Health Collaborative (2022). Awareness, Perceptions, and Literacy Surrounding Hearing Loss and Hearing Rehabilitation Among the Adult Population in the United States. Otology & neurotology : official publication of the American Otological Society, American Neurotology Society [and] European Academy of Otology and Neurotology, 43(3), e323–e330.
- Domecq, J. P., Prutsky, G., Elraiyah, T., Wang, Z., Nabhan, M., Shippee, N., Brito, J. P., Boehmer, K., Hasan, R., Firwana, B., Erwin, P., Eton, D., Sloan, J., Montori, V., Asi, N., Dabrh, A. M., & Murad, M. H. (2014). Patient engagement in research: a systematic review. BMC health services research, 14, 89
- Lin, F. R., Thorpe, R., Gordon-Salant, S., & Ferrucci, L. (2011). Hearing loss prevalence and risk factors among older adults in the United States. The journals of gerontology. Series A, Biological sciences and medical sciences, 66(5), 582–590.
- Sorkin, D. L., & Buchman, C. A. (2016). Cochlear Implant Access in Six Developed Countries. Otology & neurotology: official publication of the American Otological Society, American Neurotology Society [and] European Academy of Otology and Neurotology, 37(2), e161–e164.
Brian Taylor, AuD is the senior director of audiology for Signia and the editor of Audiology Practices. He can be contacted at
Bob Tysoe is the owner of Hearing Healthcare Marketing and Business Development. Bob can be contacted at
