
Doing More to Enhance Cognitive Health
Nancy Tye-Murray, PhD
An increasing number of audiologists are finding that new patients arrive at their clinic, not because a family member or friend has urged them to do something about their hearing loss, but rather, these (perhaps formerly reluctant) patients have read in a newspaper or heard in a news interview that hearing loss and cognitive decline go hand-in-hand, and they fear becoming victims of dementia or Alzheimer’s. Only recently have audiologists begun to think about how to expand their services to address such concerns. In this article, we will first consider the link between hearing loss and cognitive decline and then review one of the therapies that has been designed to address it.
The linkage between hearing loss and cognitive decline is indeed well-established and is believed to be multi-dimensional, which means that as audiologists, we need to take a multidimensional approach to treatment and not just end our intervention with the provision of hearing aids.
Figure 1 captures the linkage’s multidimensional nature. It begins with degenerative changes in the inner ear, such as the loss of inner and outer hair cells, the decline of spiral ganglion cells, and the atrophy of the stria vascularis. For some individuals, there is also a corresponding degenerative change in the vestibular apparatus. These changes in turn cause hearing thresholds to rise and speech discrimination to decline and may cause balance challenges. The subsequent consequences are both neurological and behavioral.
Neurologically, listening requires greater perceptual effort—as the name implies, more cognitive resources must be allocated towards decoding the acoustic signal so fewer resources are available for deciphering meaning. In addition, fewer resources are available for auditory processing. This is because neurons in the temporal cortex may have atrophied from lack of stimulation or may have been co-opted by other regions of the brain. Moreover, because of the lack of activity in one part of the brain (i.e., the temporal cortex), other regions of the brain may become less active and undergo neural atrophy as well. There may be changes in executive functions such as working memory and changes in the brain’s processing speed and attention mechanisms. These neurological changes may dovetail with changes that might be happening as a result of neurological changes associated with early dementia.
Behaviorally, listening challenges may cause a person to avoid conversations for fear of communication breakdowns or simply because conversation is too effortful with hearing loss. As a result, the person may experience social isolation and loneliness and overall decreased psychosocial wellbeing. Balance challenges may cause a person to avoid physical activity. As the person becomes increasingly isolated and physically inactive (and possibly depressed), the brain receives less stimulation, thereby exacerbating any age-related cognitive decline that might be occurring.
By giving patients hearing aids, we can possibly mollify the linkage between hearing loss and cognitive decline because the patient will be able to hear softer sounds and more high frequency sounds and will have overall better speech discrimination in both quiet and noise.
But the intervention does not have to stop with hearing aids. By using a hearing healthcare therapeutic (DTx), audiologists can begin to address some of the other factors that affect the hearing-cognition linkage.
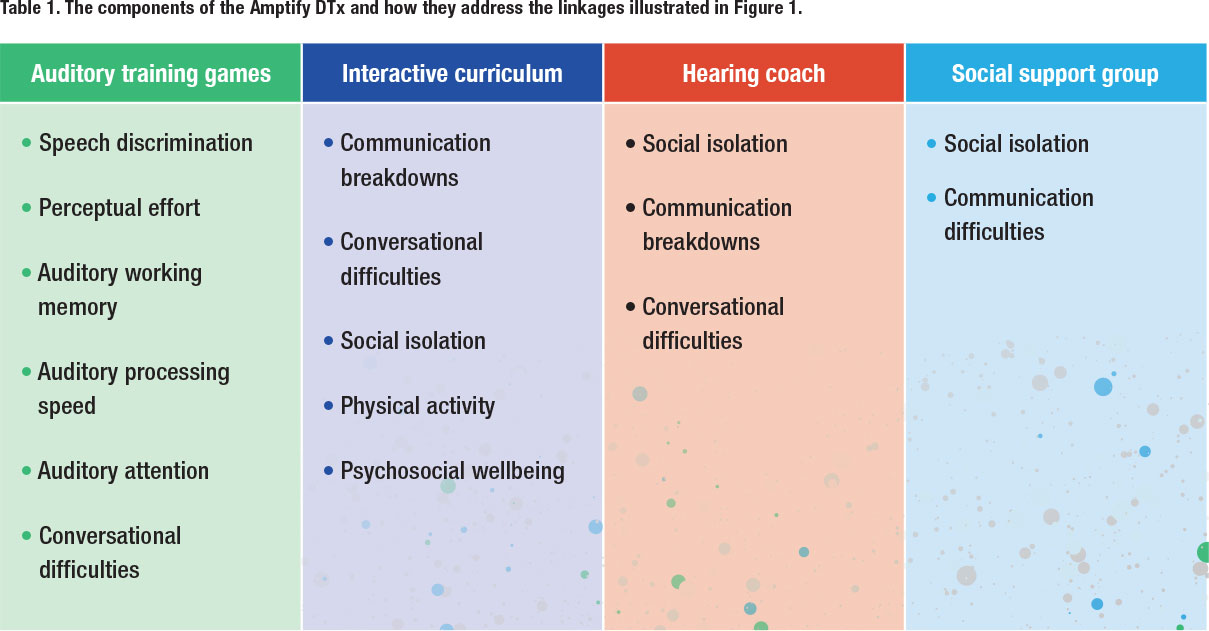
DTxs have been used to manage diabetes (Omada), asthma (Propeller Health), weight (Noom), and mental health (Headspace). A DTx is a software-based intervention for a disease and/or disorder that is clinically validated to achieve a desired outcome, and is often coupled with a medical intervention . Commonly, a DTx includes a daily, interactive curriculum, online support from a trained coach, and an online peer support group. Amptify ™ is a hearing healthcare DTx and was designed to provide follow-up care after the hearing aid fitting. The DTx includes an interactive, daily curriculum, an online hearing health coach who can be messaged 24/7, auditory training video games, and a social chat group that is overseen by the hearing health coach. Table 1 lists the four components along with the factors from Figure 1 for which they were designed to target. In sum, the Amptify DTx is comprised of the following:
 Auditory training video games. The games include animation and colorful graphic design to ensure entertainment and compliance (Figure 2). They target speech discrimination skills and exercise auditory attention, auditory processing speed, and auditory memory. The auditory training games have been shown to enhance speech discrimination (Barcroft et al., 2016), reduce perceptual effort (Sommers et al., 2015), increase listening confidence (Tye-Murray et al., 2012), and improve those communication situations that patients deem challenging (Tye-Murray et al, 2017).
Auditory training video games. The games include animation and colorful graphic design to ensure entertainment and compliance (Figure 2). They target speech discrimination skills and exercise auditory attention, auditory processing speed, and auditory memory. The auditory training games have been shown to enhance speech discrimination (Barcroft et al., 2016), reduce perceptual effort (Sommers et al., 2015), increase listening confidence (Tye-Murray et al., 2012), and improve those communication situations that patients deem challenging (Tye-Murray et al, 2017).
A daily interactive, illustrated curriculum. The curriculum engages patients through quizzes, tutorials, balance exercises, and social diaries (Figure 3). The 12- week curriculum includes such topics as preventing and rectifying communication breakdowns, structuring the listening environment to promote successful communication, nutritional tips to promote hearing health, and tinnitus management. Every week, a new balance exercise is included in the curriculum and patients are encouraged to perform the exercise by their coach. Each week, patients are also asked to reflect on and to record their social interactions via a simple three-item questionnaire embedded within the curriculum. Completing an online questionnaire can be a reactive experience, where patients will purposely engage socially so to show improvement on their “socialization feedback charts” that are part of the Amptify feedback system. The curriculum’s theme is empowerment, and patients acquire the “tools” for ensuring successful conversations.
 An online Amptify hearing health coach. Starting in the first week, users are paired with a hearing health coach, who is an audiologist and who has completed the Amptify coach training program. The coach provides support, encouragement, empathy, and hearing-related information, and works to decrease social isolation. The audiologist ensures quality-control and is available to answer questions or handle issues that might be technical in nature, as when a member might want to know about how to insert a battery into a new hearing aid.
An online Amptify hearing health coach. Starting in the first week, users are paired with a hearing health coach, who is an audiologist and who has completed the Amptify coach training program. The coach provides support, encouragement, empathy, and hearing-related information, and works to decrease social isolation. The audiologist ensures quality-control and is available to answer questions or handle issues that might be technical in nature, as when a member might want to know about how to insert a battery into a new hearing aid.
An online customized social peer support community. The Amptify team creates communities of users who share the same hearing health coach. This coach leads chats and promotes social interaction. Members are encouraged to share their experiences, find commonalities, and learn new ways to manage hearing loss through vicarious experiences. Over time, they create a friendship network.
The Amptify DTx is easy to integrate into routine clinical care and virtually all patients (and not just the I-don’t-know-what-to-do-with-them-next patients) stand to benefit from their enrollment. Amptify provides the clinics with customized clinic brochures with QR codes so their audiologists can onboard their patients. An email can also be generated to invite patients. Invitations can be integrated into the office management systems of either CounselEAR or Blueprint. Routinely including Amptify as part of the conversation a patient takes only a few minutes and can even be performed by a audiologist assistant.
Audiology can be so much more than diagnostics and listening devices. By addressing those factors that link hearing loss and cognitive decline, we can begin to provide the comprehensive hearing healthcare that we all learned about in graduate school but never had the opportunity to provide because of either time constraints or lack of effective means to provide it. The profession of audiology is changing rapidly these days, and follow-up services such as Amptify are bound to become more prevalent. n
References
- Barcroft, J., Spehar, B., Tye-Murray, N., & Sommers, M. (2016). Task-and talker-specific gains in auditory training. Journal of Speech, Language, and Hearing Research, 59(4), 862-870.
- Sommers, M. S., Tye-Murray, N., Barcroft, J., & Spehar, B. (2015). The effects of meaning-based auditory training on behavioral measures of perceptual effort in individuals with impaired hearing. Seminars in Hearing, 36(4), 263-272.
- Tye-Murray, N., Sommers, M. S., Mauzé, E., Schroy, C., Barcroft, J., & Spehar, B. (2012). Using patient perceptions of relative benefit and enjoyment to assess auditory training. Journal of the American Academy of Audiology, 23(8), 623-634.
- Tye-Murray, N., Spehar, B., Barcroft, J., & Sommers, M. (2017). Auditory training for adults who have hearing loss: A comparison of spaced versus massed practice schedules. Journal of Speech, Language, and Hearing Research, 60(8), 2337-2345.
Dr. Tye-Murray is a Professor of Audiology at Washington University in St. Louis and the founder of Amptify. She serves as Amptify’s CEO and is the lead scientist of the Amptify research team.
